A Comprehensive Breathing Myths Guide
- BioSource Faculty
- Apr 24, 2025
- 27 min read
Updated: Jun 25, 2025

Breathing ensures healthy CO2 levels. Breathing exchanges gases and regulates acid-base (pH) balance.
The respiratory system exchanges oxygen for carbon dioxide (CO2), which cells release during metabolism. CO2 regulates our physiology by increasing nitric oxide and oxygen delivery when tissues are more active. Our body uses 85-88% of CO2 in the blood to ensure a healthy acid-base balance, making gas exchange possible through the Bohr effect (Khazan, 2021). We summarize basic breathing science and debunk 14 breathing misconceptions to improve biofeedback and neurofeedback training for health and performance. These breathing myths include: 1. Carbon dioxide is a toxic waste gas we should remove. 2. We need more oxygen. 3. Oxygen intake is the primary role of breathing. 4. Take deep breaths. 5. Mouth breathing is better because it’s easier since there’s less resistance. 6. Longer exhalations during slow-paced breathing increase HRV. 7. Longer exhalations are healthier.
8. 100% oxygen saturation is better than 98%.
9. Pulse oximeters are accurate for everyone.
10. Holding your breath increases lung capacity.
11. Slow-paced breathing is healthy for everyone.
12. Abdominal breathing should feel more natural than thoracic breathing.
13. You should breathe slowly throughout the day. 14. The Wim Hof Method (WHM) involving rapid breathing and cold exposure is healthy. This post draws on Dr. Inna Khazan's extensive lectures and writing on healthy breathing. Dani S@unclebelang on Fiverr.com drew the beautiful WEBTOONs illustrating these myths.

This post also incorporates Dr. Christopher Gilbert's contributions on overbreathing.

Basic Breathing Science
pH
The abbreviation pH refers to the power of hydrogen, which is the concentration of hydrogen ions. Acidic solutions have a low pH (< 7) due to a high concentration of hydrogen ions. A neutral solution of distilled water has a pH of 7. Alkaline or basic solutions have a high pH (>7) due to a low concentration of hydrogen ions. The pH level regulates oxygen and nitric oxide release. pH graphic © AlexVector/Shutterstock.com.

Breathing Ensures Healthy CO2 Levels
The main functions of breathing are gas exchange and acid-base (pH) regulation. Respiratory system alveoli exchange oxygen for carbon dioxide (CO2) released by cells during metabolism. Alveoli are tiny, thin-walled gas exchange sacs in the lung (Fox & Rompolski, 2022). Alveolus gas exchange graphic © Designua/Shutterstock.com.

CO2
Our body uses 85-88% of blood CO2 to ensure a healthy acid-base balance to prevent our blood from becoming too acidic (acidosis) or basic (alkalosis). Breathing allows the respiratory system to maintain a blood pH level between 7.35 and 7.45 (Hopkins, Sanvictores, & Sharma, 2022). Homeostasis graphic © Designua/Shutterstock.com.

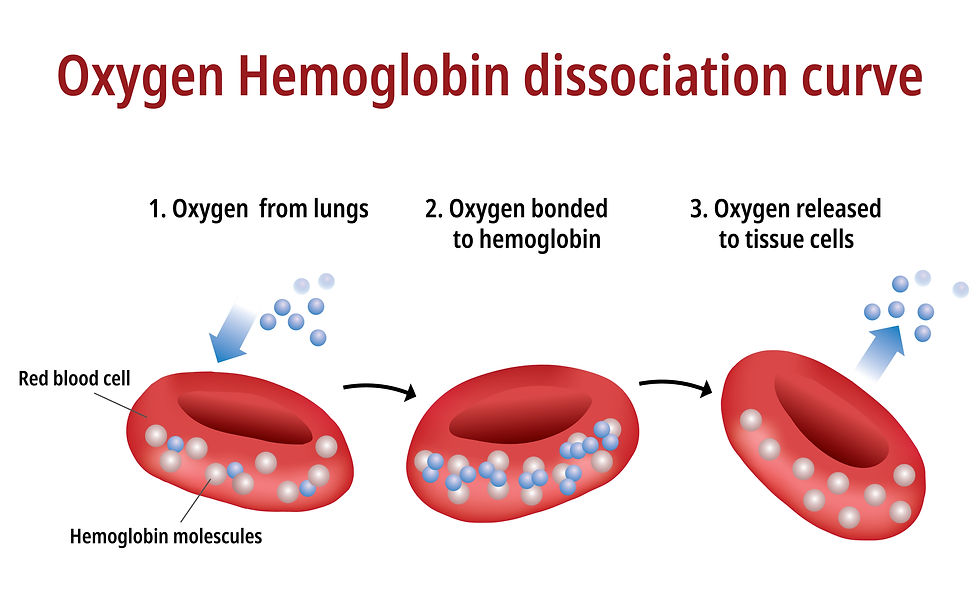
Hemoglobin
Hemoglobin molecules on red blood cells transport oxygen and nitric oxide through the bloodstream. One hemoglobin molecule can carry four oxygen or nitric oxide molecules. Oxygen and nitric oxide compete for attachment to hemoglobin's binding sites. Hemoglobin graphic © Peddalanka Ramesh Babu/Shutterstock.com.

CO2 Controls pH Levels
CO2 regulates pH levels to distribute oxygen and nitric oxide. When cells are active, they produce CO2. Aerobic respiration graphic © Designua/Shutterstock.com.

Inspiratory muscle activity (e.g., diaphragm and the external intercostal) increases metabolism. Muscles break down glucose and fatty acids to power contraction, which produces CO2 (Milic-Emili & Tyler, 1963; Swensen, 2017).
Slow-paced breathing with low tidal volumes retains more CO2 in arterial blood than when overbreathing. Tidal volume (TV) is the amount of air inhaled or exhaled during a normal breath (Fox & Rompolski, 2022).

In both cases, rising CO2 lowers blood pH (more acidic), weakening the bond between hemoglobin and oxygen and nitric oxide to support physical activity. Hemoglobin graphic © Love Employee/Shutterstock.com.

The Bohr Effect
The Bohr effect enables oxygen and nitric oxide to leave their hemoglobin carrier to enter blood vessels and cells (Riggs, 1988). Bohr effect graphic © Designua/Shutterstock.com.

Oxygen's Functions
In cells, oxygen supports mitochondrial (orange) ATP production and metabolism to support activity. Human cell graphic © Corona Borealis Studio/Shutterstock.com.

Nitric Oxide's Role
Slow-paced breathing releases more nitric oxide as blood CO2 rises and pH falls, resulting in vasodilation. Graphic is courtesy of Dr. Christopher Gilbert (2005).

Nitric oxide dilates capillaries and arterioles, increasing oxygen, nitric oxide, and nutrient delivery via blood flow. Blood vessel graphic © ALIOUI MA/Shutterstock.com.

Overbreathing
Overbreathing is a mismatch between breathing rate and depth (Khazan, 2021). This disparity may involve rapid breathing, increased tidal volume (the amount of air inhaled or exhaled during a breath), and more subtle behaviors like gasps and sighs. Overbreathing graphic © Silvia Bukovac/Shutterstock.com.

Overbreathing can reduce CO2 levels, raising blood pH (more alkaline) and reducing oxygen and nitric oxide delivery to body tissues since oxygen remains tightly bound to hemoglobin molecules (Fox & Rompolski, 2022).

Overbreathing can produce acute and chronic vasoconstriction effects and reduced delivery of oxygen and glucose to body tissues, especially the brain (Khazan, 2013). Cerebral circulation graphic © Magic mine/Shutterstock.com.

This SPECT scan created by Dr. Scott Woods shows the effect of overbreathing on brain metabolism. Darker colors represent reduced metabolism and compromised cortical functioning.

Clinicians use the Nijmegen questionnaire to screen for hyperventilation syndrome (HVS). For the general population, scores ≥ 20 have been suggested as optimal for predicting HVS, with a sensitivity of 0.91 and specificity of 0.92 (Looha et al., 2020). In asthma patients, a cutoff score of > 17 has been used to discriminate the presence of HVS, showing a sensitivity of 92.73% and specificity of 91.59% (Grammatopoulou et al., 2014). In a study involving dizzy patients, a cutoff score of 26.5 was found to be the most sensitive for diagnosing HVS (Taalot, Moaty, & Elsayed, 2019).

Why Challenge Breathing Myths?
Clients and practitioners are bombarded by scientific misinformation on social media by influencers peddling nonsense like “carbon dioxide is a toxic waste gas.” Breathing myths can reinforce dysfunctional breathing behaviors, sabotaging biofeedback and neurofeedback training. Social media graphic © Lightfield Studios/Shutterstock.com.

Myth 1. Carbon dioxide is a toxic waste gas we should remove.
CO2 is not toxic in the concentrations produced by the body under normal conditions (Tanaka, Sato, & Kasai, 2020). CO2 is crucial in the human body's respiratory and cardiovascular systems. It is a key component of the blood's buffering system, helping to maintain pH balance (Crystal, 2015). The concentration of CO2 in the blood regulates breathing rates; low levels (hypocapnia) can lead to respiratory alkalosis (increased pH), while high levels (hypercapnia) stimulate breathing to remove excess CO2, maintaining homeostasis (Ainslie & Duffin, 2009). CO2 is essential for the Bohr effect. The Bohr effect describes how the presence of CO2 facilitates the release of oxygen from hemoglobin, enhancing oxygen delivery to tissues. This effect demonstrates CO2's critical role in ensuring that oxygen is efficiently supplied to where it is most needed in the body (Malte & Lykkeboe, 2018). Our bodies require end-tidal CO2 levels of 35-45 mmHg (torr) to maintain homeostasis (Rapoport, Norman, & Goldring, 1993).

Myth 2. We need more oxygen.
Under normal conditions, most people's blood is saturated with oxygen at about 95-100% (Qadir & Tanveer, 2019).
The issue is not the amount of oxygen in the blood but how effectively the body's tissues utilize it (Jensen, 2004). This is influenced by factors like the Bohr effect, where CO2 levels help to release oxygen from hemoglobin (Malte & Lykkeboe, 2018).
Rather than needing to maximize oxygen intake, maintaining adequate levels of CO2 is crucial for efficient oxygen usage (Gaspary et al., 2024). Overbreathing expels too much CO2, leading to a condition known as hypocapnia, which can reduce blood flow to the brain and impair oxygen release by hemoglobin, paradoxically leading to symptoms of oxygen shortage (Zouboules & Day, 2019).
We do not need more oxygen! (Khazan, 2021).
Near sea level, the air healthy clients inhale contains 21% oxygen, while the air they exhale has 16% (Brenckmann et al., 2019). We only use ¼ of inhaled oxygen and don’t need more. We need to conserve CO2 by retaining 85-88% of it.

Myth 3. Oxygen intake is the primary role of breathing.
The myth that the primary role of breathing is oxygen intake oversimplifies the complex functions of the respiratory system. While obtaining oxygen is crucial to breathing, it's not the sole purpose.
Equally important to inhaling oxygen (O2) is exhaling carbon dioxide (CO2), a byproduct of cellular metabolism. Removing CO2 from the body is critical for maintaining the acid-base balance in the blood, preventing acidosis (decreased alkalinity), and ensuring that cellular processes function correctly (Lujan & DiCarlo, 2018).
Breathing plays a pivotal role in regulating the pH level of the blood. By adjusting the rate and depth of breathing, the body can control the amount of CO2 expelled, directly influencing the blood's acidity. This regulation is vital for the proper functioning of enzymes and metabolic processes (Guyenet & Bayliss, 2015). The table below shows how CO2 regulates blood pH and is redrawn from Gilbert (2005).

Breathing supports the efficient exchange of gases in the lungs, where oxygen is absorbed into the bloodstream, and CO2 is released for exhalation. This exchange is crucial for metabolic activities and energy production within cells (Hsia, 2023).

4. Take deep breaths.
The key to healthy breathing lies in its efficiency, not its depth. Efficient breathing using the diaphragm (diaphragmatic breathing), allows for optimal gas exchange in the lungs (Gosselink, 2004). The quality of the breath, involving complete oxygen and CO2 exchange, is more important than the volume of air inhaled (Pomidori et al., 2009).
Fast breathing is OK and deep breathing is OK, but not both, unless you’re exercising heavily, dumping more CO2 into the bloodstream.
Breathing deeply without maintaining the correct balance between oxygen and carbon dioxide can disrupt the body's gas equilibrium and pH (Zoccal, 2022). The physiological benefits of breathing are maximized when there's a proper balance, supporting cellular respiration and maintaining blood pH levels (Imray et al., 2003).
For some individuals, especially those with anxiety or panic disorders, taking deep breaths without proper technique or guidance can lead to hyperventilation (Han et al., 1997). This excessive breathing can decrease CO2 levels too much, potentially causing symptoms like dizziness, palpitations, or increased anxiety (Gorman et al., 1994).
Discourage typical deep breathing, where a client inhales a massive breath and inevitably exhales too quickly because this promotes overbreathing and expels too much CO2 (Khazan, 2021). Our colleague Don Moss no longer uses "deep" when coaching breathing (Moss, 2022).

Myth 5. Mouth breathing is better because it’s easier since there’s less resistance.
Mouth breathing does encounter less resistance than nose breathing.
This is due to the narrower cross-sectional area and more complex anatomy of the nasal passages, which include turbinates and mucosal surfaces that create greater frictional resistance to airflow (Haight & Cole, 1983; Elad et al., 2008). Nasal cavity graphic © gritsalak karalak/ Shutterstock.com.

Mouth breathing is fine when there’s a need for large amounts of air, such as exercising, or when the nose is stuffed.
But less resistance doesn’t always mean better.
Encourage your clients to inhale through the nostrils to filter, moisten, and warm the air. They should exhale through the mouth or nose depending on training goals and health. The nose acts as a natural filter, trapping dust, allergens, and other particulate matter before they can enter the lungs (Bjermer, 1999). Nasal passages also humidify and warm the air, protecting the respiratory tract from irritation and infection (Naclerio et al., 2007). Mouth breathing bypasses these natural defenses (Martel et al., 2020).
Inhaling through the nose releases nitric oxide, a gas that enhances the body’s ability to transport oxygen by dilating blood vessels, to the lungs. This process improves oxygen uptake in the blood, contributing to better overall cardiovascular health. Mouth breathing does not offer this benefit (Kimberly et al., 1996; Watso et al., 2023).
Chronic mouth breathing can lead to dry mouth, increasing the risk of dental decay and gum disease because saliva, which protects against bacteria and aids digestion, is reduced (Tamkin, 2020). Furthermore, the altered posture of the tongue and jaw can contribute to malformations in children, such as dental malocclusions and facial deformities (Lin et al., 2022).
Inhaling through the nose helps regulate the volume of inhaled air and maintains adequate levels of CO2 in the blood, which is necessary to efficiently release oxygen from hemoglobin to the body’s tissues (Prisca et al., 2024). Mouth breathing can lead to overbreathing and a reduction in CO2 levels, impairing oxygen delivery (LaComb et al., 2017; Tanaka, Morikawa, & Honda, 1988). Exhaling through the nose cannot be regulated in the way that pursed-lips breathing can. Exhaling through pursed lips reduces inappropriate breathing volume when the cause is emotion rather than exercise demand.
Many people favor practicing breathing by inhaling through the nose and exhaling through the mouth, so that's a compromise between the two that makes sense.

Myth 6. Longer exhalations during slow-paced breathing increase HRV.
Zachary Meehan and Fred Shaffer (2024) systematically reviewed 11 inhalation-to-exhalation (I/E) ratio HRV studies using the revised Cochrane risk-of-bias tool. They concluded that longer I/E ratios do not reliably increase HRV.

Myth 7: Longer exhalations are healthier.
We are unaware of well-controlled randomized controlled trials (RCTs) confirming the health benefits of longer exhalations. "Well-controlled" means the investigators confirmed that participants breathed at the same rates and followed inhalation-to-exhalation (IE) rate instructions. Below are searches using ChatGPT, Gemini, and Perplexity. We excluded studies that only reported on HRV changes since the best-controlled studies (Meehan & Shaffer, 2024) showed no effect.



Professionals arguing that longer exhalations are healthier and equal IE ratios are harmful have not supported their claims with evidence from randomized-controlled trials. For example, do longer exhalations lower blood pressure or blood sugar? Do equal IE ratios raise blood pressure or blood sugar? The widely-used Institute of HeartMath Coherence Coach breathing pacer has used equal IE ratios for decades without incident.
Slowly exhaling is useful for conscious regulation of breathing (Zaccaro et al., 2018), but not the same as saying it’s "healthier." Anxiety management usually benefits from intentional slow exhalation and is a common therapeutic recommendation to be used strategically (Magnon, Dutheil, & Vallet, 2021).
Individual Health Conditions: For people with respiratory conditions, such as COPD or asthma, excessively long exhalations can lead to challenges like incomplete lung emptying or increased breathing work, which might exacerbate their condition (Broeders et al., 2004; van Geffen et al., 2018).
Activity and Demand: During physical activity, the body's demand for oxygen increases, necessitating a quicker breathing rate (Harms, 2015). Longer exhalations in such scenarios can reduce oxygen intake efficiency, potentially impairing performance and leading to faster fatigue (Hasler et al., 2020). Effective breathing involves adapting to the body’s needs and balancing oxygen intake and carbon dioxide expulsion (Brinkman, Toro, & Sharma, 2023). The ideal breathing pattern varies depending on current activities, emotional state, and health conditions.

Myth 8: 100% oxygen saturation is better than 98%.
Oxygen saturation measures the percentage of hemoglobin binding sites in the bloodstream occupied by oxygen (Collins et al., 2015). Oxygen saturation between 95-98% is normal at sea level for healthy individuals. Graphic © Biology Education/ Shutterstock.com.

Saturations of 95-98% are better than 100% because “it means there’s a bit more oxygen in the bloodstream and a bit less in the tissues, which is the only place where it can do any good” (Gilbert, 2012, p. 138).
Hemoglobin graphic © Akarat Phasuran/Shutterstock.com.
Consider this analogy: A truck is delivering groceries to a grocery store, and people in the store are waiting to buy those groceries. But the truck doors are only partly open, allowing only a few groceries to be unloaded and placed on the shelves. There are plenty of groceries in the truck, but not enough groceries in the store. That’s what happens with extra-high O2 saturation. The oxygen cannot perform its function in the bloodstream; it has to be released to the issues (Gilbert, 2012, p. 138).
When SpO2 exceeds 98%, the additional oxygen is primarily dissolved in the plasma. This can produce oxidative stress, vasoconstriction, and tissue injury, especially in critically ill patients. While 100% SpO2 is not harmful in brief or healthy contexts (e.g., post-exercise recovery), in many clinical settings, 99% is preferred to avoid excessive oxygen exposure. The ideal range is 95-98%.
100% oxygen saturation is not better than 98% saturation because the additional oxygen is dissolved into the plasma, where it can harm vulnerable patients.
For most adults receiving supplemental oxygen, the preferred target oxygen saturation (SpO₂) is 94–98%, according to major clinical guidelines (O'Driscoll et al., 2017).
A lower target of 88-92% is recommended in chronic obstructive pulmonary disease (COPD) to avoid suppressing the hypoxic respiratory drive or worsening acidosis. (Echevarria et al., 2021).

Myth 9: Pulse oximeters are accurate for everyone.
Physicians use oximetry to identify patients who need supplemental oxygen (American Lung Association, 2025). Since this technology was developed using a racially non-diverse population, it should not be surprising that occult hypoxemia (undetected blood oxygen levels below 88%) was three times more likely in Black than White patients in two large cohorts (Valbuena et al., 2022). During the COVID-19 pandemic, patients of color were sent home instead of intensive care units due to inaccurate oxygen saturation measurements. Misleading pulse oximeter readings delayed treatments, increased hospitalization rates, limited access to necessary medical interventions, and exacerbated existing health disparities (Holder & Wong, 2022).

Myth 10: Holding your breath increases lung capacity.
Lung capacity is the maximum air the lungs can hold, typically measured in liters. It includes several components, such as tidal volume (air inhaled and exhaled during normal breathing) and vital capacity (the maximum air exhaled after a maximum inhalation; Delgado & Bajaj, 2023).
Total lung capacity is determined largely by genetics, age, sex, and physical conditioning, but environmental factors and overall health also influence it (Frisancho et al., 1997; Quanjer et al., 1993).
Holding your breath can increase tolerance to higher CO2 levels. It may temporarily affect how comfortably you can hold your breath (breath-holding time), but it does not increase the lung's capacity to hold air (Whitelaw, McBride, & Ford, 1985).
People know about Japanese pearl divers holding their breath for long times. It’s not an increase in lung capacity, but tolerance for hypoxia and higher CO2, plus vigorous hyperventilating before the dive to produce respiratory alkalosis. There have been deaths by drowning reported over the years in U.S. high school pools and military situations, pushing the limits of underwater swimming (Lane, 2017).
Frequent and intense breath-holding can be risky, especially without proper training and supervision. It can lead to a dangerous condition known as hypoxia (oxygen deprivation), which, in extreme cases, can cause unconsciousness, brain damage, or even death (Jewell, 2023; WebMD, 2023).

Myth 11: Slow-paced breathing is healthy for everyone.
Slow-paced breathing can be highly beneficial for stress reduction and cardiovascular health, but it is not a one-size-fits-all remedy. Its appropriateness depends on individual health conditions, activity levels, and specific situations. Personalized approaches and, in some cases, medical guidance are recommended to ensure that breathing practices are both safe and effective.
Individual Health Conditions: Slow breathing might disrupt the acid-base balance in people with metabolic disorders like diabetes or kidney disease. For respiratory disorders like asthma or COPD, disruption could result from overbreathing, but this can be avoided with expert training (British Thoracic Society, 2024).
Adaptation to Activity Levels: During physical exertion, slow breathing might not provide sufficient oxygen intake or carbon dioxide expulsion, potentially causing decreased performance and discomfort (Russo, Santarelli, & O’Rourke, 2017).
Risk of Hypoventilation: Excessively slow breathing can lead to hypoventilation, especially if the breaths are not deep enough. This can increase blood carbon dioxide levels, causing headaches, confusion, and dizziness (Jewell, 2023; Russo, Santarelli, & O’Rourke, 2017).

Myth 12: Abdominal breathing should feel more natural than thoracic breathing.
Although abdominal breathing has many health benefits and is effective for relaxation and efficient breathing, suggesting it should feel more natural than thoracic breathing for everyone is an oversimplification. Various factors influence breathing patterns, including physical structure, health conditions, activity levels, and learned behaviors (Sackner et al., 2015; Yamguti et al., 2012).
Training: Abdominal breathing can be learned and may become more natural with practice, especially in contexts like yoga or meditation. However, initially, it might not feel as natural, particularly if one has been predominantly a thoracic breather (Bahenský et al., 2021).
Physical Differences: People have different physical and anatomical structures, affecting how comfortable or natural a particular breathing style may feel. For some, thoracic breathing may feel more natural, especially during certain activities or due to their physical conditioning (Garrido-López et al., 2024; Gómez-Recio et al., 2024).
Health Conditions: Those with respiratory issues or certain medical conditions might find abdominal breathing more difficult or less natural. For example, individuals with obesity or abdominal pain may find thoracic breathing easier (Gol & Rafraf, 2021).
Activity Level: During vigorous exercise or stressful situations, thoracic breathing can feel more natural and effective in meeting the body’s increased oxygen demands. Conversely, abdominal breathing is more beneficial in calm, restful states or during relaxation and stress reduction practices (Canoy et al., 2004).

Myth 13: You should breathe slowly throughout the day.
When breathing slows excessively, the lungs do not expel enough CO2, leading to its accumulation in the bloodstream. This condition is referred to as hypercapnia. This can cause respiratory acidosis (reduced blood pH), potentially resulting in confusion, fatigue, and shortness of breath. Slow breathing could be hazardous if your client suffers from diseases that produce metabolic acidosis, like diabetes and kidney disease, or respiratory acidosis, like chronic obstructive pulmonary disease (Gallo de Moraes & Surani, 2019). Overbreathing attempts to compensate for abnormal acid-base balance and slow-paced breathing could endanger health.
Maintaining a slow breathing rate regardless of physical demands can prevent the body from properly adjusting to different activities, potentially reducing overall physical efficiency and responsiveness (Migliaccio et al., 2023). Adopting an adaptive breathing strategy that adjusts to current needs is more beneficial. For instance, employing slow breathing techniques during rest, stress, or meditation can be very beneficial, but allowing the body to increase breathing rate during exercise or excitement is crucial for optimal physiological function.

Myth 14: The Wim Hof Method (WHM) involving rapid breathing and cold exposure is healthy.
The Wim Hof Method (WHM), popularized by Wim Hof, also known as "The Iceman," involves rapid breathing techniques, cold exposure, and meditation. While it claims numerous health benefits and has garnered a substantial following, it's important to approach the method with a nuanced understanding of its potential benefits and risks.
Hyperventilation Risks: The rapid breathing aspect of the WHM can lead to hypocapnia, a state of reduced carbon dioxide in the blood, which can cause symptoms like dizziness, tingling, confusion, and even fainting (Citherlet et al., 2021).
Cold Exposure Risks: While brief cold exposure can boost the immune response and metabolism, prolonged exposure without proper acclimatization can lead to hypothermia and other cold-related injuries. Individuals with cardiovascular issues might be at higher risk when exposed to extreme cold (Ikäheimo, 2018; Zhang et al., 2014).
Medical Conditions: Individuals with certain health conditions, such as cardiovascular diseases, respiratory issues, or high blood pressure, should be cautious and consult healthcare providers before attempting the WHM (Citherlet et al., 2021; Giraldo, López, & Solà-Soler, 2023).
Lack of Scientific Consensus: Although some studies support aspects of the WHM, the research is not extensive enough to conclusively determine its purported benefits or long-term effects. More rigorous, peer-reviewed studies are needed to understand its impacts on various health aspects fully (Almahayni & Hammond, 2023).
The claim that the Wim Hof Method is universally healthy overlooks the complex interplay of individual health conditions, the risks associated with extreme practices like rapid breathing and cold exposure, and the lack of comprehensive scientific validation. While there may be benefits, they must be weighed against potential risks, especially those with underlying health issues. Anyone interested in the WHM must approach it with caution, ideally under the guidance of a healthcare professional, and to consider their personal health status and risks.

Conclusion
Biofeedback and neurofeedback training may benefit from identifying and correcting your clients' breathing myths. Breathing misconceptions can interfere with training by promoting overbreathing, ignoring your body's interoceptive feedback, and overriding your breathing reflex. Shifting to a healthy breathing pattern corrects overbreathing by conserving 85-88% of CO2 in the blood. Conserving CO2 lowers blood pH, weakens the bond between hemoglobin and oxygen, and increases nitric oxide and oxygen delivery to body tissues courtesy of the Bohr effect. Healthy breathing dilates blood vessels, slows heart rate (HR), increases respiratory sinus arrhythmia (RSA) and heart rate variability (HRV), and lowers blood pressure (BP).
Glossary
abdominal breathing: a breathing technique that involves breathing using the diaphragm rather than the upper chest muscles. As the diaphragm contracts and moves downward, the abdomen expands, allowing for fuller lung expansion and more efficient air exchange.
acidosis: a decrease in the normal alkalinity of the blood or tissues, leading to a lower pH level. It can be caused by an increase in acid production, a decrease in acid excretion, or a loss of bicarbonate, which is a base that helps neutralize acids in the body.
Bohr effect: physiological phenomenon that describes how the binding affinity of hemoglobin for oxygen is influenced by changes in pH and carbon dioxide concentration.
carbon dioxide: a gas produced by cellular metabolism, crucial for regulating breathing, maintaining blood pH balance, and facilitating oxygen delivery to tissues.
diaphragm: the dome-shaped muscle whose contraction enlarges the vertical diameter of the chest cavity and accounts for about 75% of air movement into the lungs during relaxed breathing.
effortless breathing: Erik Peper’s relaxed breathing method in which the client uses about 70% of maximum effort, attention settles below the waist, and the volume of air moving through the lungs increases. The subjective experience is that "my body breathes itself."
end-tidal CO2: the percentage of CO2 in exhaled air at the end of exhalation.
hypercapnia: a condition characterized by an abnormally high level of carbon dioxide (CO₂) in the blood.
hypocapnia: a condition characterized by abnormally low levels of carbon dioxide (CO2) in the blood, typically resulting from excessive breathing (hyperventilation). Hypocapnia can lead to symptoms such as dizziness, tingling in the limbs, confusion, and in severe cases, seizures. inhalation-to-exhalation (IE) ratio: the proportion of time spent on inhaling (breathing in) compared to exhaling (breathing out) during a breathing cycle.
inspiratory muscles: the diaphragm and external intercostals.
lung capacity: the maximum air the lungs can hold, typically measured in liters.
metabolic acidosis: a disturbance characterized by a decrease in the body's bicarbonate levels or an increase in the production of acids, leading to a reduction in the arterial blood pH below 7.35. This condition can result from increased acid production (such as ketoacidosis or lactic acidosis), reduced kidney acid secretion, or significant bicarbonate losses.
nitric oxide: signaling molecule produced in the body that promotes vasodilation, enhances blood flow, supports immune defense, and is involved in regulating pulmonary function.
overbreathing: a mismatch between breathing rate and depth. This disparity may involve rapid breathing, increased tidal volume (the amount of air exhaled during a breath), and more subtle behaviors like gasps and sighs.
oxygen saturation: a measure of the percentage of hemoglobin binding sites in the bloodstream occupied by oxygen. respiratory acidosis: a state in which decreased ventilation (hypoventilation) leads to an increase in carbon dioxide concentration and a decrease in blood pH. This condition is often due to impaired lung function, chest injuries, or diseases that affect the respiratory muscles or control of breathing.
respiratory alkalosis: a condition characterized by elevated blood pH due to excessive carbon dioxide exhalation, typically caused by hyperventilation.
thoracic breathing: breathing that primarily uses the muscles of the upper chest, with minimal engagement of the diaphragm. The chest expands and rises significantly during thoracic breathing, common during intense physical activity or acute stress. This method is less efficient regarding oxygen and carbon dioxide exchange than diaphragmatic breathing.
tidal volume (VT): the amount of air inhaled or exhaled during a normal breath.
torr: the unit of atmospheric pressure, named after Torricelli, which equals 1 millimeter of mercury (mmHg), is used to measure end-tidal CO2. Wim Hof Method: a technique developed by Wim Hof that purportedly combines specific breathing exercises, cold exposure, and meditation to improve physical and mental health. The method aims to strengthen the body's ability to withstand cold, improve respiratory control, and enhance overall well-being. However, it should be cautiously approached, especially by individuals with underlying health conditions.
References
Ainslie, P., & Duffin, J. (2009). Integration of cerebrovascular CO2 reactivity and chemoreflex control of breathing: Mechanisms of regulation, measurement, and interpretation. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology, 296(5), R1473-95. https://doi.org/10.1152/ajpregu.91008.2008
Almahayni, O., & Hammond, L. (2023). Does the Wim Hof Method have a beneficial impact on physiological and psychological outcomes in healthy and non-healthy participants? A systematic review. PLOS ONE, 19. https://doi.org/10.1371/journal.pone.0286933
American Lung Association (2025). Pulse oximetry. https://www.lung.org/lung-health-diseases/lung-procedures-and-tests/pulse-oximetry
Bahenský, P., Bunc, V., Malátová, R., Marko, D., Grosicki, G., & Schuster, J. (2021). Impact of a breathing intervention on engagement of abdominal, thoracic, and subclavian musculature during exercise, a randomized trial. Journal of Clinical Medicine, 10. https://doi.org/10.3390/jcm10163514
Bjermer, L. (1999). The nose as an air conditioner for the lower airways. Allergy, 54. https://doi.org/10.1111/j.1398-9995.1999.tb04403.x
Brenckmann, V., Ventrillard, I., Romanini, D., Jaulin, K., Calabrese, P., & Briot, R. (2019). High inhaled oxygen concentration quadruples exhaled CO in healthy volunteers monitored by a highly sensitive laser spectrometer. Scientific Reports, 9. https://doi.org/10.1038/s41598-019-48789-8
Brinkman, J. E., Toro, F., & Sharma, S. (2023). Physiology, respiratory drive. StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482414/
British Thoracic Society (2024). BTS/SIGN/NICE Joint Guideline for the Diagnosis, Monitoring and Management of Chronic Asthma. https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/
Broeders, M., Molema, J., Hop, W., Vermue, N., & Folgering, H. (2004). The course of inhalation profiles during an exacerbation of obstructive lung disease. Respiratory Medicine, 98(12), 1173-1179 . https://doi.org/10.1016/J.RMED.2004.04.010
Canoy, D., Luben, R., Welch, A., Bingham, S., Wareham, N., Day, N., & Khaw, K. (2004). Abdominal obesity and respiratory function in men and women in the EPIC-Norfolk Study, United Kingdom. American Journal of Epidemiology, 159(12), 1140-1149. https://doi.org/10.1093/AJE/KWH155
Citherlet, T., Von Roten, C., Kayser, B., & Guex, K. (2021). Acute effects of the Wim Hof breathing method on repeated sprint ability: A pilot study. Frontiers in Sports and Active Living, 3. https://doi.org/10.3389/fspor.2021.700757
Collins, J. A., Rudenski, A., Gibson, J., Howard, L., & O'Driscoll, R. (2015). Relating oxygen partial pressure, saturation and content: The haemoglobin-oxygen dissociation curve. Breathe (Sheffield, England), 11(3), 194–201. https://doi.org/10.1183/20734735.001415h
Crystal, G. (2015). Carbon dioxide and the heart: Physiology and clinical implications. Anesthesia & Analgesia, 121, 610–623. https://doi.org/10.1213/ANE.0000000000000820
Delgado, B. J., & Bajaj, T. (2023). Physiology, lung capacity. StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK541029/
Echevarria, C., Steer, J., Wason, J., & Bourke, S. (2021). Oxygen therapy and inpatient mortality in COPD exacerbation. Emergency Medicine Journal: EMJ, 38(3), 170–177. https://doi.org/10.1136/emermed-2019-209257
Elad, D., Naftali, S., Rosenfeld, M., & Wolf, M. (2008). Physical stresses at the air–mucus interface of the human nasal cavity during normal breathing. Respiratory Physiology & Neurobiology, 163(1-3), 128–132. https://doi.org/10.1016/j.resp.2008.04.019
Fox, S. I., & Rompolski, K. (2022). Human physiology (16th ed.). McGraw-Hill.
Fried, R. (1987). The hyperventilation syndrome: Research and clinical treatment. John Hopkins University Press.
Fried, R., & Grimaldi, J. (1993). The psychology and physiology of breathing. Springer.
Frisancho, A., Frisancho, H., Albalak, R., Villain, M., Vargas, E., & Soria, R. (1997). Developmental, genetic, and environmental components of lung volumes at high altitude. American Journal of Human Biology, 9(2), 191–203. https://doi.org/10.1002/(SICI)1520-6300(1997)9:2<191::AID-AJHB5>3.0.CO;2-3
Gallo de Moraes, A., & Surani, S. (2019). Effects of diabetic ketoacidosis in the respiratory system. World Journal of Diabetes, 10(1), 16–22. https://doi.org/10.4239/wjd.v10.i1.16
Garrido-López, G., Rueda, J., Navarro, E., Juan, A., & Bastir, M. (2024). Evaluation of thorax diameter changes through trunk morphology and different running intensities. Applied Sciences, 14(17), 7600. https://doi.org/10.3390/app14177600
Gaspary, J., Edgar, L., Lopes, L., Rosa, C., & Siluk, J. (2024). Translational insights into the hormetic potential of carbon dioxide: From physiological mechanisms to innovative adjunct therapeutic potential for cancer. Frontiers in Physiology, 15, 1415037. https://doi.org/10.3389/fphys.2024.1415037
Gilbert, C. (2005). Better chemistry through breathing: The story of carbon dioxide and how it can go wrong. Biofeedback, 33(3), 100-104.
Giraldo, B., López, D., & Solà-Soler, J. (2023). Analysis of heart rate variability during the performance of the Wim Hof method in healthy subjects. 2023 45th Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), 1-4. https://doi.org/10.1109/EMBC40787.2023.10340840
Gol, R., & Rafraf, M. (2021). Association between abdominal obesity and pulmonary function in apparently healthy adults: A systematic review. Obesity Research & Clinical Practice. https://doi.org/10.1016/j.orcp.2021.06.011
Gómez-Recio, M., Bastir, M., LoMauro, A., Aliverti, A., & Beyer, B. (2024). Three-dimensional geometric morphometric shape analysis of chest wall kinematics in different breathing conditions. Royal Society Open Science, 11. https://doi.org/10.1098/rsos.240548
Gorman, J., La, P., Coplan, J., Martinez, J., Lennon, S., Goetz, R., Ross, D., & Klein, D. (1994). Anxiogenic effects of CO2 and hyperventilation in patients with panic disorder. The American Journal of Psychiatry, 151(4), 547-553. https://doi.org/10.1176/AJP.151.4.547
Gosselink, R. (2004). Breathing techniques in patients with chronic obstructive pulmonary disease (COPD). Chronic Respiratory Disease, 1, 163 - 172. https://doi.org/10.1191/1479972304cd020rs
Grammatopoulou, E., Skordilis, E., Georgoudis, G., Haniotou, A., Evangelodimou, A., Fildissis, G., Katsoulas, T., & Kalagiakos, P. (2014). Hyperventilation in asthma: A validation study of the Nijmegen Questionnaire – NQ. Journal of Asthma, 51, 839 - 846. https://doi.org/10.3109/02770903.2014.922190
Guyenet, P., & Bayliss, D. (2015). Neural control of breathing and CO2 homeostasis. Neuron, 87, 946-961. https://doi.org/10.1016/j.neuron.2015.08.001
Haight, J. S., & Cole, P. (1983). The site and function of airway resistance in the human nose. Archives of Otolaryngology, 109(8), 544–546. https://doi.org/10.1001/archotol.1983.00800220030010
Han, J., Stegen, K., Simkens, K., Cauberghs, M., Schepers, R., Bergh, O., Clement, J., & Woestijne, K. (1997). Unsteadiness of breathing in patients with hyperventilation syndrome and anxiety disorders. The European Respiratory Journal, 10(1), 167-176 . https://doi.org/10.1183/09031936.97.10010167
Harms, C. A, (2015). Breathing in exercise: Battle of the sexes. The Journal of Physiology, 593(8), 1763. https://doi.org/10.1113/jphysiol.2015.270249 https://doi.org/10.1113/JP270249
Hasler, E., Saxer, S., Schneider, S., Furian, M., Lichtblau, M., Schwarz, E., Bloch, K., & Ulrich, S. (2020). Effect of breathing oxygen-enriched air on exercise performance in patients with chronic obstructive pulmonary disease: Randomized, placebo-controlled, cross-over trial. Respiration, 99, 213 - 224. https://doi.org/10.1159/000505819
Holder, A. L., & Wong, A. I. (2022). The big consequences of small discrepancies: Why racial differences in pulse oximetry errors matter. Critical Care Medicine, 50(2), 335–337. https://doi.org/10.1097/CCM.0000000000005447
Hopkins, E., Sanvictores, T., & Sharma, S. (2022). Physiology, acid base balance. StatPearls. StatPearls Publishing. PMID: 29939584
Hsia, C. (2023). Tissue perfusion and diffusion and cellular respiration: Transport and utilization of oxygen. Seminars in Respiratory and Critical Care Medicine, 44, 594 - 611. https://doi.org/10.1055/s-0043-1770061
Imray, C., Walsh, S., Clarke, T., Tiivas, C., Hoar, H., Harvey, T., Chan, C., Forster, P., Bradwell, A., & Wright, A. (2003). Effects of breathing air containing 3% carbon dioxide, 35% oxygen or a mixture of 3% carbon dioxide/35% oxygen on cerebral and peripheral oxygenation at 150 m and 3459 m. Clinical Science, 104(3), 203-210. https://doi.org/10.1042/CS20020102
Jensen, F. (2004). Red blood cell pH, the Bohr effect, and other oxygenation-linked phenomena in blood O2 and CO2 transport. Acta Physiologica Scandinavica, 182(3), 215-227. https://doi.org/10.1111/j.1365-201X.2004.01361.x
Jewell, T. (2023). How to train to hold your breath longer safely. healthline. https://www.healthline.com/health/holding-your-breathhttps://www.healthline.com/health/holding-your-breath
Jewell, T. (2023). Hypercapnia: What is it and how is it treated? healthline. https://www.healthline.com/health/hypercapnia
Khazan, I. (2019). A guide to normal values for biofeedback. In D. Moss & F. Shaffer (Eds.). Physiological recording technology and applications in biofeedback and neurofeedback (pp. 2-6). Association for Applied Psychophysiology and Biofeedback.
Khazan, I. (2019). Biofeedback and mindfulness in everyday life: Practical solutions for improving your health and performance. W. W. Norton & Company.
Khazan, I. Z. (2013). The clinical handbook of biofeedback: A step-by-step guide for training and practice with mindfulness. John Wiley & Sons, Ltd.
Kimberly, B., Nejadnik, B., Giraud, G., Holden, W., & Holden, W. (1996). Nasal contribution to exhaled nitric oxide at rest and during breathholding in humans. American Journal of Respiratory and Critical Care Medicine, 153(2), 829-836. https://doi.org/10.1164/AJRCCM.153.2.8564139
Ikäheimo, T. (2018). Cardiovascular diseases, cold exposure and exercise. Temperature, 5, 123 - 146. https://doi.org/10.1080/23328940.2017.1414014
LaComb, C., Tandy, R., Lee, S., Young, J., & Navalta, J. (2017). Oral versus nasal breathing dring moderate to high intensity submaximal aerobic exercise. International Journal of Kinesiology and Sports Sciences, 5, 8-16. https://doi.org/10.7575//AIAC.IJKSS.V.5N.1P.8
Lane, J. D. (2017). Drowning deaths from unsupervised breath holding: Separating necessary training from unwarranted risk. Military Medicine, 182(1-2), 1471–1473. https://doi.org/10.7205/MILMED-D-16-00246
Lin, L., Zhao, T., Qin, D., Hua, F., & He, H. (2022). The impact of mouth breathing on dentofacial development: A concise review. Frontiers in Public Health, 10, 929165. https://doi.org/10.3389/fpubh.2022.929165
Looha, M., Masaebi, F., Abedi, M., Mohseni, N., & Fakharian, A. (2020). The optimal cut-off score of the Nijmegen Questionnaire for diagnosing hyperventilation syndrome using a Bayesian model in the absence of a gold standard. Galen Medical Journal, 9, e1738 - e1738. https://doi.org/10.31661/gmj.v9i0.1738
Lujan, H., & DiCarlo, S. (2018). An acid-base "shock and awe" demonstration: The bad breath test. Advances in Physiology Education, 42(3), 462-463. https://doi.org/10.1152/advan.00049.2018
Magnon, V., Dutheil, F., & Vallet, G. (2021). Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Scientific Reports, 11. https://doi.org/10.1038/s41598-021-98736-9
Malte, H., & Lykkeboe, G. (2018). The Bohr/Haldane effect: A model-based uncovering of the full extent of its impact on O2 delivery to and CO2 removal from tissues. Journal of Applied Physiology, 125(3), 916-922. https://doi.org/10.1152/japplphysiol.00140.2018
Martel, J., Ko, Y., Young, J., & Ojcius, D. (2020). Could nasal nitric oxide help to mitigate the severity of COVID-19? Microbes and Infection, 22, 168 - 171. https://doi.org/10.1016/j.micinf.2020.05.002
Meehan, Z. M., & Shaffer, F. (2024). Do longer exhalations increase HRV during slow-paced breathing? Applied Psychophysiology and Biofeedback. https://doi.org/10.1007/s10484-024-09637-2 Migliaccio, G. M., Russo, L., Maric, M., & Padulo, J. (2023). Sports performance and breathing rate: What is the connection? A narrative review on breathing strategies. Sports, 11(5), 103. https://doi.org/10.3390/sports11050103htt s://doi.org/10.3390/sports11050103 Milic‐Emili, J., & Tyler, J. (1963). Relation between work output of respiratory muscles and end-tidal CO2 tension. Journal of Applied Physiology, 18(3), 497-504. https://doi.org/10.1152/JAPPL.1963.18.3.497 Naclerio, R., Pinto, J., Assanasen, P., & Baroody, F. (2007). Observations on the ability of the nose to warm and humidify inspired air. Rhinology, 45(2), 102-111. PMID: 17708456
O'Driscoll, B. R., Howard, L. S., Earis, J., & Mak, V. (2017). British Thoracic Society guideline for oxygen use in adults in healthcare and emergency settings. BMJ Open Respiratory Research, 4(1), e000170. https://doi.org/10.1136/bmjresp-2016-000170
Pomidori, L., Campigotto, F., Amatya, T., Bernardi, L., & Cogo, A. (2009). Efficacy and tolerability of yoga breathing in patients with chronic obstructive pulmonary disease: A pilot study. Journal of Cardiopulmonary Rehabilitation and Prevention, 29, 133–137. https://doi.org/10.1097/HCR.0b013e31819a0227 Prisca, E., Pietro, C., Anja, K., Laura, S., Sarina, H., Dominic, K., Sabina, G., & Matthias, W. (2024). Improved exercise ventilatory efficiency with nasal compared to oral breathing in cardiac patients. Frontiers in Physiology, 15. https://doi.org/10.3389/fphys.2024.1380562
Qadir, M., & Tanveer, M. (2019). The connection of normal blood oxygen level and eye blinking. Mathews Journal of Emergency Medicine, 4(1), 32. https://doi.org/10.30654/MJEM.10032
Quanjer, P., Tammeling, G., Cotes, J., Pedersen, O., Peslin, R., & Yernault, J. (1993). Lung volumes and forced ventilatory flows. European Respiratory Journal, 6, 40-45. https://doi.org/10.1183/09041950.005s1693.ttps://doi.org/10.30654/mjem.10032
Rapoport, D., Norman, R., & Goldring, R. (1993). CO2 homeostasis during periodic breathing: Predictions from a computer model. Journal of Applied Physiology, 75(5), 2302-2309. https://doi.org/10.1152/JAPPL.1993.75.5.2302 Riggs, A. (1988). The Bohr effect. Annual Review of Physiology, 50, 181-204. https://doi.org/10.1146/ANNUREV.PH.50.030188.001145 Russo, M. A., Santarelli, D. M., & O'Rourke, D. (2017). The physiological effects of slow breathing in the healthy human. Breathe, 13(4), 298–309. https://doi.org/10.1183/20734735.009817 Sackner, M., Gonzalez, H., Jenouri, G., & Rodríguez, M. (2015). Effects of abdominal and thoracic breathing on breathing pattern components in normal subjects and in patients with chronic obstructive pulmonary disease. The American Review of Respiratory disease, 130(4), 584-587. https://doi.org/10.1164/ARRD.1984.130.4.584 Swenson, E. (2017). Carbon dioxide elimination by cardiomyocytes: A tale of high carbonic anhydrase activity and membrane permeability. Acta Physiologica, 221. https://doi.org/10.1111/apha.12922 Talaat, H., Moaty, A., & Elsayed, M. (2019). Arabization of Nijmegen questionnaire and study of the prevalence of hyperventilation in dizzy patients. Hearing, Balance and Communication, 17, 182 - 188. https://doi.org/10.1080/21695717.2019.1590989 Tamkin J. (2020). Impact of airway dysfunction on dental health. Bioinformation, 16(1), 26–29. https://doi.org/10.6026/97320630016026
Tanaka, Y., Morikawa, T., & Honda, Y. (1988). An assessment of nasal functions in control of breathing. Journal of Applied Physiology, 65(4), 1520-1524. https://doi.org/10.1152/JAPPL.1988.65.4.1520
Tanaka, T., Sato, H., & Kasai, K. (2020). Lethal physiological effects of carbon dioxide exposure at high concentration in rats. Legal Medicine, 47, 101746. https://doi.org/10.1016/j.legalmed.2020.101746 Valbuena, V. S. M., Seelye, S., Sjoding, M. W., Valley, T. S., Dickson, R. P., Gay, S. E., Claar, D., Prescott, H. C., & Iwashyna, T. J. (2022). Racial bias and reproducibility in pulse oximetry among medical and surgical inpatients in general care in the Veterans Health Administration 2013-19: Multicenter, retrospective cohort study. BMJ (Clinical research ed.), 378, e069775. https://doi.org/10.1136/bmj-2021-069775 van Geffen, W. H., Slebos, D.-J., & Kerstjens, H. A. M. (2015). Hyperinflation in COPD exacerbations. The Lancet Respiratory Medicine, 3(12), e43-e44. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600%2815%2900459-2/fulltext
Watso, J., Cuba, J., Boutwell, S., Moss, J., Bowerfind, A., Fernandez, I., Cassette, J., May, A., & Kirk, K. (2023). Abstract P342: Acute nasal breathing lowers blood pressure and increases parasympathetic contributions to heart rate variability in young adults. Hypertension. https://doi.org/10.1161/hyp.80.suppl_1.p342
WebMD (2023). Is it safe to hold your breath? https://www.webmd.com/a-to-z-guides/is-it-safe-to-hold-your-breath
Whitelaw, W. A., McBride, B., & Ford, G. T. (1987). Effect of lung volume on breath holding. Journal of Applied Physiology, 62(5), 1962–1969. https://doi.org/10.1152/jappl.1987.62.5.1962
Yamaguti, W., Claudino, R., Neto, A., Chammas, M., Gomes, A., Salge, J., Moriya, H., Cukier, A., & Carvalho, C. (2012). Diaphragmatic breathing training program improves abdominal motion during natural breathing in patients with chronic obstructive pulmonary disease: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 93(4), 571-577. https://doi.org/10.1016/j.apmr.2011.11.026
Zaccaro, A., Piarulli, A., Laurino, M., Garbella, E., Menicucci, D., Neri, B., & Gemignani, A. (2018). How breath-control can change your life: A systematic review on psycho-physiological correlates of slow breathing. Frontiers in Human Neuroscience, 12. https://doi.org/10.3389/fnhum.2018.00353 Zelano, C., Jiang, H., Zhou, G., Arora, N., Schuele, S., Rosenow, J., & Gottfried, J. A. (2016). Nasal respiration entrains human limbic oscillations and modulates cognitive function. Journal of Neuroscience, 36(49), 12448. https://doi.org/10.1523/JNEUROSCI.2586-16.2016
Zhang, X., Zhang, S., Wang, C., Wang, B., & Guo, P. (2014). Effects of moderate strength cold air exposure on blood pressure and biochemical indicators among cardiovascular and cerebrovascular patients. International Journal of Environmental Research and Public Health, 11, 2472 - 2487. https://doi.org/10.3390/ijerph110302472
Zoccal, D. (2022). Past questions, present results, future perspectives: Interacting chemosensitive areas and the hypercapnic ventilatory response. The Journal of Physiology, 600. https://doi.org/10.1113/JP283142https. The doi.org/10.1523/JNEUROSCI.2586-16.2016
Zouboules, S., & Day, T. (2019). The exhausting work of acclimating to chronically elevated CO2. The Journal of Physiology, 597. https://doi.org/10.1113/JP277491
Support Our Friends










This is exactly what I am teaching at Conspire Health. Many thanks to Inna and Dr. Peter Litchfield for educating and inspiring me.