Interpreting the Raw EEG: Fast Alpha
- Fred Shaffer
- Jun 18, 2025
- 12 min read
Updated: Sep 9, 2025

What Is Fast Alpha?
Fast alpha refers to electroencephalographic activity within the upper end of or beyond the conventional alpha frequency band.
Traditionally, alpha is defined as a sinusoidal rhythm between 8 and 12 Hz, most prominent over the occipital cortex during relaxed wakefulness with eyes closed. However, not all individuals conform neatly to this boundary. Some display dominant alpha peaks in the 11–13 Hz range, which are physiologically normal and may reflect either a faster intrinsic oscillatory frequency or a distinct alpha sub-band.
A smaller subset of EEG recordings reveal activity in the 18–19 Hz range that appears as a harmonic—an exact multiple—of a lower primary alpha generator, most commonly 9–9.5 Hz. This 2:1 frequency relationship is not a second rhythm per se but a byproduct of waveform asymmetry and neural resonance within the thalamocortical loop.
Fast alpha in the 11–13 Hz range is especially common in individuals with high levels of cognitive functioning, efficient information processing, or enhanced attentional control. This has been supported by studies linking faster alpha with working memory performance, sensory integration, and age-related changes in cortical synchronization (Grandy et al., 2013; Klimesch, 1999). Fast alpha is also associated with anxiety and hypervigilance (Klimesch et al., 2007; Oathes et al., 2008; Putman, 2011; Thibodeau et al., 2006). Our colleague, John S. Anderson reported that his patients with fast alpha experience sleep issues, "driven" behavior, and a breakdown of cognitive and physiological systems.
Increased alpha frequency may also be associated with heightened emotional and psychological drive, which could contribute to greater achievement in various life domains. However, this remains a subject of ongoing debate, with differing perspectives in the literature. Based on John S. Anderson's clinical observations, fast alpha activity appears to correlate with success-oriented behaviors, though it may also be linked to potential physical and mental health vulnerabilities in later life. He cautioned that these correlations may not be universal.
Faster alpha frequencies are correlated with higher intelligence (Clark et al., 2004; Grandy et al., 2013; Posthuma et al., 2001).
Grandy et al. (2013) conducted a large-scale study of healthy adults and found that:
“Individuals with higher IAPF demonstrated better cognitive performance across a wide range of intelligence tests.”
Posthuma et al. (2001) found a genetic correlation between IAPF and intelligence:
“There is a significant positive genetic correlation between the individual alpha frequency and IQ, suggesting common genetic influences.” John S. Anderson cautions that the observed correlation between alpha frequency and intelligence may be partially attributable to heritable factors; however, it may also reflect learned behavior, as children often emulate parental behavioral patterns. Consequently, this association could arise from environmental and physiological mechanisms related to parenting style, expectations, and early cognitive stimulation. Faster alpha rhythms may allow for more efficient information gating and synchrony in cortical networks. Faster cycles might permit quicker information integration and updating, facilitating superior cognitive performance.
The 18–19 Hz variant, in contrast, is not directly tied to cognitive state but instead reflects the dynamic behavior of the alpha oscillator under certain structural and functional constraints of the neural generator. Recognizing both types of fast alpha is essential for EEG professionals, as they occupy a gray zone between what is considered normal rhythmic background and what might otherwise be mistaken for pathological beta activity.
What Is Its Morphology?
The morphology of fast alpha shares many surface features with classical alpha rhythms: it is sinusoidal, rhythmic, and demonstrates waxing and waning amplitude patterns. When in the 11–13 Hz range, the waveforms are typically low to moderate in amplitude, symmetrical across hemispheres, and maximally expressed over the parieto-occipital regions. They tend to have a sharper peak and shorter cycle length than slower alpha, but still maintain the overall smooth appearance characteristic of physiologic alpha activity. Their spatial distribution often matches that of the individual’s dominant alpha frequency and remains reactive to state changes, including eye opening and alerting stimuli.
In contrast, the 18–19 Hz harmonic often exhibits a more flattened amplitude profile and may appear less sustained. These waveforms are generally brief, appearing most clearly immediately after eye closure and disappearing within a few seconds.
They may occur in trains of several hundred milliseconds or emerge as transient events without forming a continuous rhythm. This alpha squeak graphic © The Atlas of Adult Electroencephalography.
Their detection is most reliable in frequency-domain displays, such as fast Fourier transform (FFT) spectrograms, where they appear as secondary peaks precisely double the frequency of the main alpha generator. While morphologically similar to low-amplitude beta activity, they are distinguished by their reactivity and posterior location. Importantly, these harmonics do not propagate across electrode sites in the manner of epileptiform discharges or sleep spindles, nor do they evolve in morphology across time.
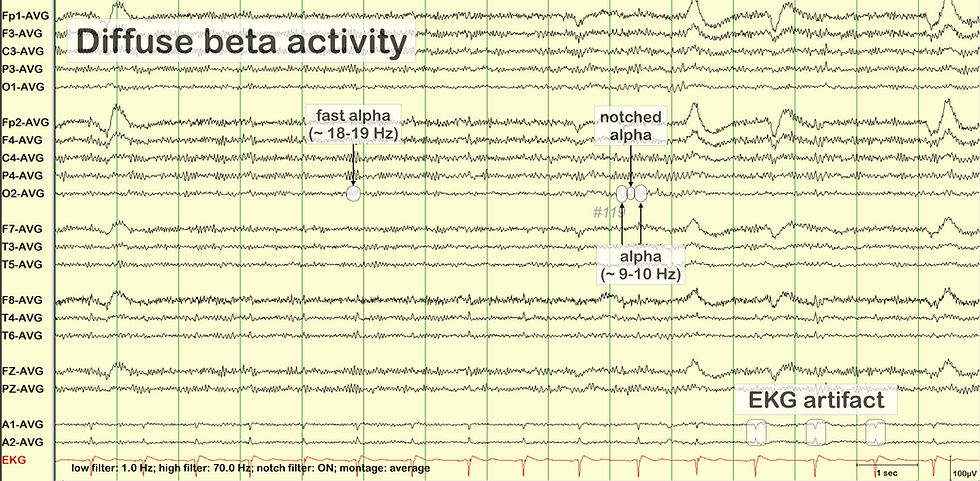
Raw EEG Analysis
The EEG segment above illustrates a complex but non-pathological combination of background rhythms and artifacts. The most striking global feature is the presence of diffuse beta activity. This fast activity, greater than 13 Hz, is visible across much of the record but appears most pronounced in anterior and midline derivations such as F3-AVG, F4-AVG, and FZ-AVG. It is characterized by relatively low amplitude and consistent distribution, and in the absence of focal enhancement, asymmetry, or reactivity loss, this diffuse beta is most likely benign. Such patterns can be seen in states of alertness, in individuals with high cortical arousal, or in those using certain medications like benzodiazepines or stimulants. However, no pharmacologic history is provided here, and the pattern lacks the frontally dominant spindling seen in sedative-induced beta excess.
Within the posterior channels, a well-formed alpha rhythm in the 9–10 Hz range is observed, particularly in P3-AVG, P4-AVG, O1-AVG, and O2-AVG. This rhythm shows typical features of a posterior dominant rhythm (PDR): it is symmetric, reactive, and appears during relaxed wakefulness. Notably, the morphology of this alpha rhythm is occasionally interrupted by waveform notching—a brief reduction in amplitude or distortion of the waveform contour—most clearly seen in P4-AVG. This phenomenon, known as notched alpha, is often the result of overlapping spectral components or transient interference from harmonics or background noise. It does not indicate pathology and should not be mistaken for epileptiform activity or phase reversal.
Above the baseline alpha, there is a higher-frequency component in the range of 18–19 Hz, briefly visible in the same posterior leads. This fast alpha activity likely represents a harmonic of the underlying alpha generator, most consistent with a second harmonic arising from a base frequency near 9.5 Hz. The appearance of such harmonics suggests a strong and regular thalamocortical alpha oscillator. Although the 18–19 Hz component is subtle, its symmetry, posterior localization, and transient nature support its classification as a benign harmonic rather than pathological beta or drug effect.
Another clear feature in the recording is the presence of EKG artifact. This is especially visible in the A1-AVG and A2-AVG channels, where periodic waveforms align with the QRS complexes seen in the lower red EKG tracing. These signals likely reflect either direct conduction of cardiac electrical signals or volume-conducted mechanical pulsations, and they should not be mistaken for sharp transients or epileptiform discharges.
Inexperienced professionals might misinterpret several features in this record. The diffuse beta activity could be erroneously labeled as abnormal fast activity suggestive of encephalopathy or medication effect, when in fact it falls within the range of benign fast beta seen in alert individuals. The fast alpha harmonic, especially if seen out of context, could be confused with low-voltage beta spindling or interpreted as a separate pathological rhythm. Similarly, the notched alpha might be mistaken for epileptiform discharge due to its irregular shape. Finally, the EKG artifact could be misread as lateralized sharp transients if its temporal alignment with the EKG channel is not carefully checked.
Overall, this EEG segment reflects a physiologically normal pattern composed of diffuse beta activity, posterior alpha with harmonic structure, and identifiable EKG artifact. It highlights the importance of correlating waveform morphology, spatial distribution, and reactivity to correctly interpret findings and avoid false-positive conclusions.
What Causes Fast Alpha?
Fast alpha rhythms arise from multiple neurophysiological mechanisms, depending on the frequency range and context. For activity in the 11–13 Hz band, the prevailing hypothesis attributes it to variation in thalamocortical resonance—that is, the frequency at which thalamic pacemaker cells synchronize with cortical relay neurons in a feedback loop governing rhythmic cortical activity. Individuals differ in the structural and functional integrity of this loop, with factors such as genetic background, neural conduction velocity, white matter microstructure, and developmental age all influencing the natural oscillatory frequency. Fast alpha is more frequently observed in adolescents and young adults and may decline or slow slightly with aging. Furthermore, research has shown that peak alpha frequency (PAF) is heritable and stable across cognitive states, making it a potential biomarker of central nervous system efficiency and cognitive performance (Grandy et al., 2013).
The 18–19 Hz harmonic variant, on the other hand, is not an independent rhythm with its own generator but rather a mathematical artifact of the primary alpha waveform.
Most brain oscillations deviate from ideal sine waves and exhibit non-linear distortion due to the asymmetry of the depolarizing and repolarizing phases of neuronal firing. This asymmetry leads to the generation of harmonics—multiples of the fundamental frequency—that appear as smaller amplitude peaks in spectral analyses. In well-formed and highly synchronized alpha rhythms, this effect becomes particularly pronounced. Thus, the presence of a visible second harmonic at 18–19 Hz typically indicates a strong, symmetric, and stable alpha generator. It does not reflect beta activity, nor does it arise from a separate cortical source.
Which Misinterpretation Must Be Ruled Out?
The most pressing clinical issue surrounding fast alpha is its frequent misclassification, particularly when spectral peaks in the 18–19 Hz range are erroneously interpreted as beta spindling, pathological fast activity, or early signs of drug effects.
This misinterpretation may lead to unnecessary concern or misdiagnosis, particularly in patients undergoing evaluations for altered mental status, epilepsy, or drug intoxication. Beta spindling—especially in the frontocentral regions—is commonly seen in patients taking benzodiazepines, barbiturates, or certain antiepileptic drugs. It is typically characterized by sustained trains of rhythmic 18–30 Hz activity that are non-reactive to eye opening and often asymmetric or frontal in distribution. In contrast, alpha harmonics are brief, symmetric, posterior, and reactive. Confusing the two could result in the erroneous attribution of a drug-induced effect or cortical irritability.
Another potential misinterpretation is mistaking fast alpha for sleep spindles, especially if the harmonic appears during drowsiness. However, sleep spindles typically occur in the 12–15 Hz range, are maximal at central sites, and exhibit a waxing–waning envelope that differs from the parieto-occipital topography of harmonics. Clinicians must also distinguish fast alpha from pathologic beta excess, such as that seen in metabolic encephalopathies, which tend to be diffuse, high amplitude, and lack spatial or reactive features.
Careful attention to distribution, reactivity, and context—as well as correlation with medication history and clinical state—is essential for accurate interpretation. Visual inspection of both the raw EEG and its frequency representation can help prevent erroneous conclusions.
How Should a Clinician Report Fast Alpha?
When fast alpha is observed, it should be described with precision and clinical neutrality. The report should specify the rhythm’s frequency, amplitude, location, symmetry, and response to state changes such as eye opening or cognitive activation. For example, in the case of 11–13 Hz alpha, a clinician might write: "The background consists of a posterior dominant rhythm at 12.5 Hz, symmetric and reactive to eye opening, with no pathological features."
When harmonics at 18–19 Hz are observed, the report should reflect that these are physiologic extensions of the alpha generator rather than independent rhythms: "Following eye closure, a brief 18–19 Hz harmonic of the posterior dominant rhythm is noted over occipital leads. This activity is symmetric, reactive, and consistent with a normal variant. No epileptiform activity or pathological beta is observed."
Including this level of detail not only prevents misinterpretation by other clinicians but also supports consistency in clinical documentation and longitudinal comparisons. When appropriate, referencing the likely harmonic origin can clarify that the finding does not imply cortical hyperexcitability or drug-related changes.
What We Wish Clinicians Knew About Fast Alpha
There remains a gap in understanding among many generalists and even some EEG professionals regarding the nature and significance of fast alpha, particularly its 18–19 Hz harmonic form. Clinicians may instinctively categorize all activity above 13 Hz as beta and, by extension, associate it with either pharmacologic effects or hyperarousal. Yet this overlooks the dynamic behavior of neural oscillators, especially the thalamocortical circuits responsible for alpha generation, which frequently produce harmonics due to waveform asymmetry.
We wish clinicians better appreciated that alpha harmonics are a signature of stability, not instability. Their presence should be reassuring, indicating a well-synchronized rhythm capable of producing nonlinear spectral effects.
Furthermore, we wish more emphasis were placed on reactivity and topography rather than absolute frequency when judging the clinical significance of faster activity. Harmonic alpha should not be mistaken for beta spindling, and higher-frequency PDRs (e.g., 12–13 Hz) should not be dismissed as abnormal when they are reactive and posteriorly dominant.
Finally, we wish EEG reports included more explicit identification of harmonics when present, especially in qEEG contexts where 18–19 Hz peaks may otherwise be flagged as “excess beta.” A simple note clarifying the harmonic origin of such peaks can preempt misinterpretation and promote better interprofessional communication. As understanding of individual differences in alpha architecture advances—especially with growing interest in peak alpha frequency as a biomarker—recognizing fast alpha and its harmonics becomes not only a technical detail but a marker of analytic sophistication.
Key Takeaways
Fast alpha in the 11–13 Hz range is a normal variant of the posterior dominant rhythm and often reflects higher cognitive efficiency and individual peak frequency variation.
Alpha harmonics at 18–19 Hz are not independent rhythms but nonlinear byproducts of strong 9–9.5 Hz alpha generators; they are benign and reactive.
Misinterpretation risk is high; clinicians must distinguish fast alpha harmonics from pathological beta spindling, drug effects, and encephalopathic fast activity based on distribution, reactivity, and symmetry.
Spectral analysis is useful for identifying harmonics, but visual inspection of raw EEG is essential to avoid false-positive qEEG interpretations of “excess beta.”
Reporting fast alpha should include frequency, location, reactivity, and clarification of harmonic origin when present to ensure accurate clinical interpretation.

Glossary
alpha harmonics: rhythmic activity that appears at exact multiples of the primary alpha frequency, typically around 18–19 Hz, arising from nonlinear waveform distortion rather than a separate neural generator.
alpha rhythm: a regular oscillation in the 8–12 Hz range, most prominent over occipital regions during relaxed wakefulness with eyes closed, reflecting thalamocortical synchronization.
amplitude: the voltage height of an EEG waveform, usually measured in microvolts (µV), reflecting the strength of cortical activity.
asymmetry: a difference in amplitude or waveform morphology between corresponding regions of the two hemispheres; in alpha harmonics, the rhythm is typically symmetric.
beta spindling: sustained, rhythmic 18–30 Hz activity commonly seen in the frontal or central regions, often associated with benzodiazepine or barbiturate use.
cognitive performance: mental processes such as attention, memory, and processing speed, which have been associated with variations in peak alpha frequency.
cycle length: The duration of one full oscillation of a waveform; shorter cycle lengths correspond to higher frequencies such as fast alpha.
depolarization: a phase in neuronal firing when the membrane potential becomes less negative, contributing to the shape and frequency of EEG waveforms.
drowsiness: A transitional state between wakefulness and sleep that can affect EEG rhythms, sometimes resulting in misinterpretation of fast alpha as sleep spindles.
epileptiform activity: pathological EEG discharges such as spikes or sharp waves, which differ from benign rhythms like fast alpha in morphology and behavior.
eye closure response: the appearance or enhancement of alpha rhythm following the voluntary closing of the eyes, reflecting cortical disengagement from visual input.
fast alpha: EEG activity in the 11–13 Hz range (or harmonics near 18–19 Hz), representing individual variations in alpha rhythm or nonlinear extensions of the primary alpha generator.
frequency: The number of waveform cycles per second, measured in hertz (Hz); in EEG, frequency defines the classification of rhythms such as alpha, beta, or theta.
frontal beta: fast EEG activity over the frontal cortex, often associated with alertness or medication effects; distinct from posterior alpha harmonics.
harmonic distortion: a mathematical consequence of waveform asymmetry, resulting in the generation of multiples of a base frequency, such as alpha harmonics.
microvolt (µV): A unit of electrical potential used to measure EEG amplitude; one microvolt equals one millionth of a volt.
Nonlinear oscillator: a system, such as the thalamocortical circuit, that produces waveforms with asymmetric shapes, leading to the appearance of harmonic frequencies.
occipital region: the posterior part of the scalp, overlying the visual cortex, where alpha rhythms and their harmonics are typically maximal.
peak alpha frequency (PAF): the individual-specific frequency at which alpha activity is strongest; used as a marker of cognitive performance and neural efficiency.
posterior dominant rhythm (PDR): the most prominent rhythmic activity in the alpha band seen over occipital regions during eye closure in awake individuals.
raw EEG: the unprocessed, time-domain EEG trace viewed during clinical interpretation; essential for distinguishing harmonics from true beta activity.
reactivity: the responsiveness of an EEG rhythm to physiological or environmental changes, such as eye opening or mental tasks; a key feature in identifying normal variants.
sleep spindle: a burst of rhythmic 12–15 Hz activity occurring during Stage 2 sleep, usually maximal over central regions and morphologically distinct from fast alpha.
spectral analysis: the transformation of EEG signals into the frequency domain (e.g., via FFT), used to identify rhythmic components and harmonics.
symmetry: the similarity of EEG features across both hemispheres; normal alpha and its harmonics are typically symmetric.
thalamocortical loop: a neural circuit connecting the thalamus and cortex, responsible for generating and maintaining rhythmic oscillations such as the alpha rhythm.
waveform morphology: the shape and structure of EEG waveforms, including smoothness, sharpness, and duration, which aid in distinguishing benign from pathological patterns.
References
Grandy, T. H., Werkle-Bergner, M., Chicherio, C., Schmiedek, F., Lövdén, M., & Lindenberger, U. (2013). Individual alpha peak frequency is related to latent factors of general cognitive abilities. NeuroImage, 79, 10–18. https://doi.org/10.1016/j.neuroimage.2013.04.059
Klimesch, W. (1999). EEG alpha and theta oscillations reflect cognitive and memory performance: A review and analysis. Brain Research Reviews, 29(2–3), 169–195. https://doi.org/10.1016/S0165-0173(98)00056-3
Niedermeyer, E., & da Silva, F. L. (2005). Electroencephalography: Basic principles, clinical applications, and related fields (5th ed.). Lippincott Williams & Wilkins.
Pfurtscheller, G., & Lopes da Silva, F. H. (1999). Event-related EEG/MEG synchronization and desynchronization: Basic principles. Clinical Neurophysiology, 110(11), 1842–1857. https://doi.org/10.1016/S1388-2457(99)00141-8
Tatum, W. O. (2014). Handbook of EEG interpretation (2nd ed.). Demos Medical Publishing. https://doi.org/10.1891/9781617052133
About the Author

Fred Shaffer earned his PhD in Psychology from Oklahoma State University. He earned BCIA certifications in Biofeedback and HRV Biofeedback. Fred is an Allen Fellow and Professor of Psychology at Truman State University, where has has taught for 50 years. He is a Biological Psychologist who consults and lectures in heart rate variability biofeedback, Physiological Psychology, and Psychopharmacology. Fred helped to edit Evidence-Based Practice in Biofeedback and Neurofeedback (3rd and 4th eds.) and helped to maintain BCIA's certification programs.
Support Our Friends










Another brilliant article by Fred Shaffer! This is especially important, because most clinicians, not having an engineering degree, don't understand the concept of harmonics arising from irregular shaped sine waves.