5-Min Science: Are Mitochondria the Cell's Motherboard?
- Fred Shaffer
- May 23, 2025
- 17 min read
Updated: Aug 1, 2025

Introduction
The conventional depiction of mitochondria as the mere “powerhouses” of the cell—though historically foundational—is now insufficient in light of recent scientific developments.
Originating from a mid-20th-century analogy, this label emphasized their role in generating adenosine triphosphate (ATP) through oxidative phosphorylation. Yet, Dr. Martin Picard, a professor at Columbia University, has catalyzed a paradigmatic shift, urging the scientific community to embrace a broader, integrative view of mitochondria as dynamic information-processing centers—akin to cellular motherboards. His synthesis of empirical findings and conceptual insights, articulated in a recent article and podcast with Scientific American, forms the basis of this essay.
We will extend his thesis by integrating new findings from neurophysiology and cognitive electrophysiology, especially relating to alpha oscillations, mitochondrial health, and systemic brain function. These updates not only refine our understanding of mitochondrial versatility but establish their centrality in cognitive and neurological health, underscoring the role of mitochondrial integrity in sustaining alpha peak frequency power—a biomarker of cognitive efficiency and neural synchrony.
Rethinking the Powerhouse Analogy
Traditionally, mitochondria have been defined by their size, structure, and biochemical function. Mitochondria graphic © Julien Tromeur/Shutterstock.com.
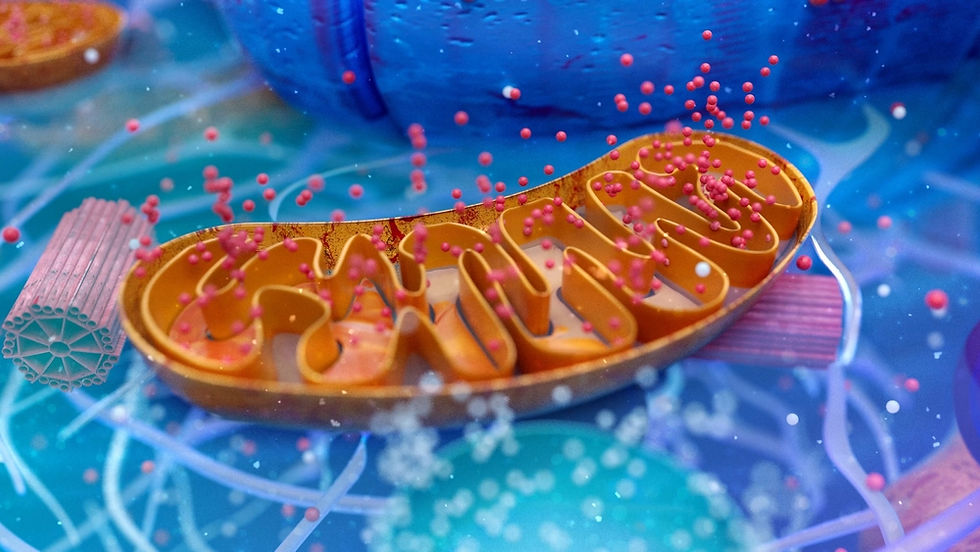
These double-membraned organelles, derived from symbiotic bacteria approximately 1.5 billion years ago, catalyze ATP production, enabling cellular processes to unfold. However, new insights show that this model is too reductionist. Mitochondria also orchestrate gene expression, regulate intracellular calcium levels, manage oxidative stress, initiate apoptosis, and even produce hormones that act within and beyond the cell.
Their role in neuroenergetics is particularly critical, especially in maintaining alpha oscillations—brainwaves in the 8–12 Hz frequency range associated with attention, memory, and sensorimotor processing. When alpha amplitude declines, clinicians often find the underlying issue is mitochondrial dysfunction. In this way, mitochondria influence both micro-level cellular health and macro-level network synchrony.
Emerging research reveals that mitochondria can synthesize and release steroid-like molecules and other metabolites that function as intracellular and paracrine signals. These hormone-like substances influence gene expression, inflammation, and systemic physiological states. In some tissues, mitochondria have been shown to contribute to the production of cortisol through local interactions and estrogenthe energetic status: should energy fall below a critical threshold, apoptotic pathways are activateds, implicating them in broader endocrine regulation.
Mitochondrial-derived signaling molecules, such as mitochondrial-derived peptides (MDPs), including humanin and MOTS-c, further demonstrate how these organelles can exert endocrine-like effects on metabolism, stress response, and even aging pathways. Thus, mitochondria communicate not only through local interactions but also through systemic biochemical messengers that resemble hormonal signaling, positioning them as active participants in cellular and organismal regulation.
Recent laboratory evidence, including that from Picard’s group, challenges the notion that mitochondria are passive and static. His team observed the unexpected alignment of cristae—the folded membranes within mitochondria responsible for ATP generation—across neighboring mitochondria. This behavior suggests that mitochondria function in social, networked clusters rather than in isolation, capable of inter-organelle communication and perhaps even electromagnetic synchrony. Analogous to how musical instruments in an orchestra must be harmonized for a coherent performance, mitochondria may align structurally and energetically to maintain cellular rhythm and integrity.
Mitochondria as Information Processors
Picard’s conceptual leap reframes mitochondria as computational hubs. In this model, they monitor internal and external signals—metabolic substrates, hormonal cues, redox states—and integrate this data to determine cellular responses. This is not dissimilar to a computer’s motherboard, where central processing coordinates various hardware functions.
For example, during synaptic activity, mitochondria are recruited to terminals to meet the energy demand of neurotransmitter cycling and ion flux. ATP generated at these sites powers sodium-potassium pumps, calcium sequestration, and vesicle recycling. Moreover, mitochondria determine cell fate by assessing energetic status: should energy fall below a critical threshold, apoptotic pathways activate via cytochrome c and caspase cascades. In the brain, these decisions have profound implications for plasticity, learning, and resilience.
This computational view is supported by research into alpha peak frequency power, which reflects the synchrony of the thalamocortical network. Alpha rhythms emerge from coordinated feedback loops between the pulvinar and reticular nuclei of the thalamus and cortical columns. Maintaining this rhythm requires a steady supply of ATP, and disruptions—particularly due to impaired oxidative phosphorylation—manifest as attenuated alpha power. These electrophysiological changes, now measurable via EEG, correlate with diminished cognitive function, memory lapses, and emotional dysregulation. Thus, alpha activity becomes an accessible readout of mitochondrial efficiency.
Evidence of Sociality: Cristae Alignment and Electromagnetic Fields
Perhaps the most visually striking evidence of mitochondrial intelligence comes from observations of cristae alignment across neighboring mitochondria. Picard’s laboratory captured electron microscopy images showing parallel cristae structures extending between adjacent mitochondria—a behavior inconsistent with standard thermodynamic models. These alignments may be driven by biophysical fields, including potential electromagnetic interactions, though this remains speculative. Nonetheless, such findings suggest a layer of mitochondrial behavior that transcends chemistry, entering the domain of systems coordination.
If mitochondria synchronize via bioelectromagnetic cues, this could explain how large-scale neural oscillations like alpha waves are regulated at the cellular level. Dysfunctional mitochondria disrupt this synchrony by generating excess reactive oxygen species (ROS), reducing ATP output, and impairing calcium buffering. These disruptions reverberate through neural circuits, weakening alpha oscillations and increasing vulnerability to neurodegenerative conditions. The analogy of the neural orchestra is apt: when mitochondria falter, the volume of the performance—the alpha wave amplitude—drops, signaling a loss of internal coherence.
From Cells to Self: The Energetic Basis of Health
The consequences of mitochondrial dysfunction are not confined to isolated cells; they scale up to affect entire networks and, by extension, subjective experience. Diseases like Alzheimer’s, chronic fatigue syndrome, and major depression often present with reduced alpha power, serving as biomarkers of deeper energetic crises. Mitochondrial failure to meet neuronal energy demands leads to impaired synaptic transmission, reduced neuroplasticity, and increased neuroinflammation. Microglia, the immune cells of the brain, respond to mitochondrial damage by releasing pro-inflammatory cytokines such as TNF-α and IL-6, further depressing alpha oscillations.
Environmental stressors—including mold-derived mycotoxins, heavy metals, and chronic stress—exacerbate these issues. Mycotoxins, such as ochratoxin A, compromise mitochondrial enzymes, impairing ATP synthesis and increasing ROS production. This biochemical disturbance triggers microglial activation, creating a neuroinflammatory feedback loop. The result is a global suppression of alpha rhythms, cognitive fog, fatigue, and mood dysregulation. As clinicians encounter resistant alpha training cases in neurofeedback, such underlying mitochondrial impairments increasingly demand integrative interventions.
Mental Health and Metabolic Psychiatry
Recent evidence increasingly implicates mitochondrial dysfunction as a significant contributor to the pathophysiology of both neurodegenerative disorders and schizophrenia. These complex conditions, while distinct in their clinical manifestations, appear to share underlying cellular energy deficits and oxidative stress pathways linked to compromised mitochondrial health. Research has further solidified these connections, highlighting specific mechanisms and potential therapeutic avenues.
Mitochondrial Dysfunction in Neurodegenerative Disorders
Mitochondria are crucial for neuronal health due to the brain's high energy demand. In neurodegenerative diseases such as Alzheimer's disease (AD), Parkinson's disease (PD), Huntington's disease (HD), and Amyotrophic Lateral Sclerosis (ALS), disruptions in mitochondrial function are consistently observed. Recent studies emphasize that mitochondrial impairment can be an early event, potentially serving as a biomarker and therapeutic target (Yusuf et al., 2023). Key aspects of this dysfunction include impaired energy metabolism, particularly defects in the oxidative phosphorylation (OXPHOS) system, which leads to reduced ATP production and increased generation of reactive oxygen species (ROS), causing oxidative stress (Ma et al., 2025).
In Alzheimer's disease, recent reviews highlight that mitochondrial dysfunction manifests as morphological abnormalities (e.g., swelling, cristae distortion), an imbalance in mitochondrial fission and fusion leading to excessive fragmentation, impaired axonal transport of mitochondria, defective mitophagy (the process of removing damaged mitochondria), and mtDNA damage due to oxidative stress (Gao et al., 2025; Kaur et al., 2025). These defects contribute to insufficient energy supply to neurons and exacerbate neurodegeneration (Gao et al., 2025).
For Parkinson's disease, mitochondrial dysfunction is a well-established hallmark, contributing to increased oxidative stress and impaired protein clearance systems (Maka et al., 2025). This is evident in both genetic forms, linked to genes like PINK1 and Parkin , which are crucial for mitochondrial quality control, and non-genetic forms, where environmental toxins can inhibit mitochondrial complex I activity (Maka et al., 2025; Abuarab et al., 2023). Dopaminergic neurons, which are primarily affected in PD, are particularly vulnerable due to their high bioenergetic needs (Abuarab et al., 2023).
Huntington's disease research has shown that the mutant huntingtin protein (mutHTT) impairs mitochondrial quality control and network dynamics, predisposing cells to pathogenic mtDNA mutations, even in peripheral tissues like skeletal muscle (Neueder et al., 2024). This lifelongsuch as PINK1 and ParkintHTT leads to mtDNA instability and impaired mitochondrial biogenesis and function, with evidence suggesting that longer CAG repeats (characteristic of HD) correlate with more severe mitochondrial phenotypes (Huntington Study Group, 2024; Neueder et al., 2024). Additionally, impaired transport of mitochondria within striatal neurons has been observed in HD models (Huntington Study Group, 2024).
In amyotrophic lateral sclerosis (ALS), recent research using CRISPR and stem cell models has identified mitochondrial dysfunction as a common early denominator across different ALS-causing gene mutations, occurring even before other overt signs of cellular disease (Schweingruber et al., 2025; Stockholm University, 2025; Technology Networks, 2025). These early issues include problems within the mitochondria themselves and in their transport to neuronal processes where energy is critically needed (Schweingruber et al., 2025; Stockholm University, 2025). Studies on sporadic ALS patients also confirm a reduction in the function of mitochondrial respiratory chain complexes, particularly Complex I and II (Škrobot et al., 2024).
Mitochondrial Dysfunction in Schizophrenia
The brain's high energy demand also makes mitochondrial function critical in psychiatric disorders like schizophrenia. Recent literature continues to build the case for OXPHOS dysfunction as a significant biological feature in schizophrenia, affecting not just a single enzymatic component but broader mitochondrial function (González-Domínguez et al., 2025). While impairment of Complex I has long been noted, alterations in other OXPHOS complexes are also being reported (González-Domínguez et al., 2025). These bioenergetic deficits, which may arise during early postnatal brain development, can disrupt neuronal metabolism and synaptic signaling, contributing to the disorder's characteristic disturbances (González-Domínguez et al., 2025).
Evidence suggests that these mitochondrial abnormalities in schizophrenia can lead to oxidative stress, apoptosis, and synaptic deterioration (González-Domínguez et al., 2025). Furthermore, some research suggests the potential utility of mitochondrial transplantation as a therapeutic strategy, although its effects can be complex and context-dependent. This is illustrated in rat models of schizophrenia, where transplantation had beneficial effects but could be detrimental in healthy controls, highlighting the need for careful consideration of the existing mitochondrial state. The question of whether mitochondrial dysfunctions are a cause or a consequence in schizophrenia remains a key area of investigation, often described as a "chicken-and-egg" dilemma (González-Domínguez et al., 2025).
In summary, the latest evidence reinforces the critical role of mitochondrial dysfunction across a spectrum of severe brain disorders. Common themes include impaired energy production, increased oxidative stress, altered mitochondrial dynamics, and defects in quality control mechanisms. These findings not only enhance the understanding of disease pathogenesis but also highlight mitochondria as a promising target for novel diagnostic and therapeutic interventions for neurodegenerative conditions and schizophrenias.
Metabolic Psychiatry
Metabolic psychiatry considers many psychiatric disorders as expressions of impaired bioenergetics. Emerging research demonstrates that mitochondrial-targeted interventions, such as ketogenic diets and mitochondrial-supportive supplements, can restore alpha power and ameliorate psychiatric symptoms. Ketones serve as alternative energy substrates, enhancing mitochondrial respiration and reducing ROS load. The brain’s energy landscape is thereby stabilized, enabling improved neural synchrony.
These findings resonate with Picard’s work, reinforcing the concept that mitochondrial vitality underpins mental resilience. In EEG research, increases in alpha power following metabolic interventions confirm the centrality of mitochondria in supporting cognitive and emotional function. The alpha peak frequency not only indexes internal brain coherence but also offers a measurable endpoint for evaluating treatment efficacy in integrative psychiatry.
The Evolutionary Origin of Mitochondrial Intelligence
The story of mitochondrial evolution underscores their significance. Once free-living bacteria, mitochondria were engulfed by host cells in a process known as endosymbiosis. This event laid the foundation for multicellular complexity by enabling efficient energy generation and intercellular communication. Mitochondria retain their own DNA, which is maternally inherited, and continue to act semi-autonomously within cells. Their evolutionary history reflects a transition from independence to interdependence—a theme echoed in their modern role as regulators of cellular and systemic coherence.
Mitochondrial dynamics—continuous cycles of fusion and fission—allow these organelles to adapt to cellular demands, isolate damaged components, and sustain network integrity. Disruptions in these dynamics contribute to conditions like autism spectrum disorder and intellectual disability. Hence, mitochondrial morphology and behavior are not incidental but central to neurodevelopmental and cognitive outcomes.
Conclusion: Toward an Energetic Model of Life
Martin Picard’s reconceptualization of mitochondria as cellular motherboards integrates molecular biology, electrophysiology, and systems neuroscience. Far from static powerhouses, mitochondria emerge as dynamic, intelligent regulators of cellular life. They shape the energetic landscape of neurons, orchestrate genetic and synaptic function, and mediate immune responses. Their health and functionality are directly linked to measurable EEG phenomena—most notably, alpha peak frequency power.
As research deepens, therapeutic opportunities expand. Photobiomodulation (PBM) and hyperbaric oxygen therapy (HBOT) exemplify cutting-edge approaches to enhancing mitochondrial function. PBM activates cytochrome c oxidase, improving oxidative phosphorylation, while HBOT increases oxygen saturation, supporting ATP synthesis and reducing inflammation. Combining these therapies with neurofeedback offers a multifaceted strategy to restore alpha rhythm integrity and cognitive health. This convergence of mitochondrial science and clinical practice heralds a future where brain health is no longer assessed or treated in isolation but through the lens of energetic coherence and cellular vitality.
Key Takeaways
Mitochondria as master regulators: Mitochondria are not merely energy producers but orchestrate complex cellular processes, including gene expression, apoptosis, calcium regulation, communication, and synaptic function, especially in neurons.
Alpha peak frequency reflects mitochondrial health: Alpha oscillations (8–12 Hz), measurable via EEG, serve as biomarkers of mitochondrial efficiency, cognitive capacity, and systemic neural synchrony.
Mitochondrial dysfunction impairs neural coherence: Disruptions in mitochondrial energy output and oxidative balance suppress alpha power and contribute to neurodegenerative and psychiatric disorders.
Environmental and inflammatory stressors compromise brain function: Exposures to mold toxins, heavy metals, or chronic stress impair mitochondrial function and amplify neuroinflammation, further dampening alpha wave activity.
Integrative therapies offer multilevel support: Interventions like photobiomodulation, hyperbaric oxygen therapy, and ketogenic diets enhance mitochondrial performance and may restore healthy alpha oscillations and cognitive function.

Glossary
alpha oscillations: rhythmic brainwaves in the 8–12 Hz frequency range associated with relaxed wakefulness and cognitive processing.
alpha peak frequency: the dominant frequency within the alpha range, used as a biomarker for cognitive efficiency and neural synchrony.
Alzheimer's disease (AD): a progressive brain disorder that slowly destroys memory and thinking skills and, eventually, the ability to carry out the simplest tasks. It is the most common cause of dementia in older adults. AD is characterized by the formation of abnormal protein deposits in the brain, specifically amyloid plaques and tau tangles, which lead to the loss of neurons and their connections. Symptoms typically begin with difficulty remembering recent events and gradually worsen to include problems with language, decision-making, judgment, and changes in personality and behavior. amyotrophic lateral sclerosis (ALS): a progressive neurodegenerative disease that affects nerve cells (motor neurons) in the brain and the spinal cord. Motor neurons reach from the brain to the spinal cord and from the spinal cord to the muscles throughout the body. The progressive degeneration of these motor neurons in ALS eventually leads to their death. When the motor neurons die, the ability of the brain to initiate and control muscle movement is lost. Consequently, ALS leads to muscle weakness, paralysis, and eventually respiratory failure. Early symptoms can include muscle twitches, weakness in a limb, or slurred speech. The disease typically does not impair a person's senses or cognitive abilities in most cases, though some individuals may develop frontotemporal dementia apoptosis: programmed cell death regulated by intracellular signals to maintain tissue health and remove damaged cells.
apoptotic pathways: regulated intracellular signaling cascades initiated by stress or damage that lead to programmed cell death, primarily involving the release of cytochrome c from mitochondria and activation of caspases to dismantle the cell in an orderly manner.
ATP (adenosine triphosphate): the primary energy currency of the cell, produced mainly by mitochondria through oxidative phosphorylation.
calcium buffering: the regulation of intracellular calcium concentrations to ensure proper cell signaling and prevent toxicity.
caspase cascades: a series of proteolytic enzymes activated during apoptosis to dismantle cellular components.
cristae: infolded structures of the inner mitochondrial membrane where components of the electron transport chain are located, crucial for ATP production through oxidative phosphorylation.
cytochrome c: a mitochondrial protein that, when released into the cytosol, initiates the apoptotic pathway.
cytokines: signaling proteins secreted by immune cells that mediate inflammation and immune responses.
electron transport chain: a mitochondrial process that transfers electrons through membrane proteins to generate ATP.
EEG (electroencephalography): a technique for recording electrical activity in the brain, used to analyze brainwave patterns.
endosymbiosis: an evolutionary process where one cell engulfs another, leading to a mutualistic relationship, as seen in the origin of mitochondria.
estrogen: a group of steroid hormones primarily responsible for the development and regulation of the female reproductive system and secondary sexual characteristics.
fusion and fission: mitochondrial processes that enable adaptation by merging or splitting to maintain function and quality control.
humanin: a mitochondrial-derived peptide that plays a protective role against cellular stress and has been implicated in aging and metabolic regulation.
hyperbaric oxygen therapy (HBOT): a treatment that delivers pure oxygen under pressure to enhance tissue oxygenation and mitochondrial function.
Huntington's disease (HD): an inherited neurodegenerative disorder that causes the progressive breakdown of nerve cells in the brain. It has a broad impact on a person's functional abilities and usually results in movement, cognitive (thinking), and psychiatric disorders. The hallmark motor symptom is chorea—involuntary, jerky, dance-like movements. Cognitive decline often involves difficulties with focus, planning, and recall, while psychiatric symptoms can include depression, anxiety, irritability, and obsessive-compulsive behaviors. HD is caused by a mutation in the HTT gene, leading to an abnormal huntingtin protein that damages neurons.
inter-organelle communication: the exchange of signals, metabolites, or structural coordination between different organelles within a cell, enabling integrated cellular responses and contributing to processes like energy regulation, apoptosis, and intracellular signaling.
ketogenic diet: a high-fat, low-carbohydrate diet that increases ketone production, supporting mitochondrial metabolism.
ketones: water-soluble molecules produced in the liver from fatty acids during periods of low carbohydrate intake, serving as an alternative energy source for the brain and supporting mitochondrial function.
microglia: immune cells in the brain responsible for responding to injury and regulating neuroinflammation.
mitochondria: organelles within cells that generate energy, regulate calcium, mediate apoptosis, and coordinate cellular signaling. mitochondrial-derived peptides (MDPs): small signaling proteins produced by mitochondria that regulate metabolism, stress responses, and cellular protection mechanisms.
mitochondrial dynamics: the continuous morphological changes mitochondria undergo through fusion and fission to meet cellular demands.
mitochondrial dysfunction: impaired performance of mitochondria, often resulting in energy deficits, oxidative stress, and disease.
motherboard: a central circuit board in electronic devices that coordinates and regulates communication between components; in biology, it metaphorically refers to mitochondria's integrative role in processing signals, distributing energy, and orchestrating cellular function.
MOTS-c: a mitochondrial-derived peptide that influences metabolism, insulin sensitivity, and cellular stress responses, playing a role in energy homeostasis and age-related health conditions.
mycotoxins: toxic secondary metabolites produced by certain molds that can impair mitochondrial function, disrupt cellular metabolism, and contribute to neuroinflammation and cognitive dysfunction.
neuroenergetics: the study of how energy production and consumption within neurons supports brain function, including processes like synaptic transmission, neural oscillations, and cognitive performance, primarily governed by mitochondrial activity.
neurofeedback: a therapeutic technique that uses real-time EEG data to help individuals regulate their own brain activity.
neuroinflammation: inflammatory response within the brain, commonly involving activated microglia and associated with neurodegenerative conditions.
oxidative phosphorylation: the process by which mitochondria generate ATP by transferring electrons through the electron transport chain.
Parkinson's disease (PD): a chronic and progressive neurodegenerative disorder that primarily affects the motor system, leading to symptoms such as tremors (shaking, often in a hand or fingers), bradykinesia (slowness of movement), limb rigidity (stiffness), and gait and balance problems. These symptoms result from the loss of dopamine-producing neurons in a specific area of the brain called the substantia nigra. Non-motor symptoms, including cognitive impairment, depression, sleep problems, and loss of smell, are also common.
photobiomodulation (PBM): a therapy using red or near-infrared light to stimulate mitochondrial activity and promote healing.
phosphorylation: the chemical process of adding a phosphate group to a molecule, often catalyzed by enzymes, which is essential for regulating protein function and producing cellular energy through ATP generation in mitochondria.
pro-inflammatory cytokines: signaling proteins released by immune cells that promote inflammation, commonly elevated in response to infection, injury, or cellular stress, and implicated in neurodegenerative and psychiatric conditions through their effect on neural function and mitochondrial health.
reactive oxygen species (ROS): highly reactive molecules formed during oxygen metabolism that can cause cellular damage if not regulated.
redox state: the balance between oxidants and antioxidants in cells, influencing mitochondrial signaling and stress responses.
sodium-potassium pump: a membrane protein that uses ATP to exchange sodium and potassium ions, essential for neural activity.
steroid hormones: a class of hormones derived from cholesterol that includes estrogen, testosterone, and cortisol, which regulate a wide range of physiological functions including metabolism, inflammation, and reproduction.
synapse: the junction between neurons where electrical or chemical signals are transmitted.
synaptic plasticity: the capacity of synapses to strengthen or weaken over time, crucial for learning and memory.
testosterone: a steroid hormone primarily responsible for the development of male reproductive tissues and secondary sexual characteristics, also playing a role in muscle mass, mood, and energy regulation.
thalamocortical loops: neural circuits connecting the thalamus and cortex, involved in generating and regulating rhythmic brain activity.
TNF-α (tumor necrosis factor-alpha): a cytokine involved in systemic inflammation and implicated in neuroinflammatory conditions.
References
Abuarab, N., Ganaie, M. A., Jan, M., & Jameel, I. (2023). Significance of mitochondrial dysfunction in the pathogenesis of Parkinson's Disease. Future Biology and Medicine, 29(1), 36. https://doi.org/10.31083/j.fbl2901036
Babiloni, C., Barry, R. J., Valenzuela, M., et al. (2021). Electroencephalographic rhythms as biomarkers for neurodegenerative disorders: A review. Neurobiology of Aging, 98, 222–237.
Bartolome, F., & Abramov, A. Y. (2013). Mitochondrial dysfunction and neuronal calcium signaling in neurodegeneration. Frontiers in Cellular Neuroscience, 7, 100.
Brini, M., Cali, T., Ottolini, D., & Carafoli, E. (2014). Neuronal calcium signaling: Function and dysfunction. Cellular and Molecular Life Sciences, 71(15), 2787–2814. https://doi.org/10.1007/s00018-013-1550-7
Efrati, S., & Ben-Jacob, E. (2014). Reflections on the neurotherapeutic effects of hyperbaric oxygen. Expert Review of Neurotherapeutics, 14(3), 233–236. https://doi.org/10.1586/14737175.2014.885835 Finsterer, J. (2004). Epilepsy in mitochondrial disorders. Epilepsy Research, 60(2–3), 161–175.
Fischer, F., Hamann, A., & Osiewacz, H. D. (2020). Mitochondrial quality control: An integrated network of pathways. Trends in Biochemical Sciences, 45(3), 179–190. https://doi.org/10.1016/j.tibs.2019.12.008
Gao, S., Liu, Z., Zhang, Q., Han, X., Liu, C., & Wang, J. (2025). Mitochondrial dysfunction in Alzheimer's disease: a key frontier for future targeted therapies. Frontiers in Aging Neuroscience, 16, 1355850. https://doi.org/10.3389/fnagi.2024.1355850
González-Domínguez, A., Martín-Hernández, D., Garcia-Bueno, B., & Bioque, M. (2025). Mitochondrial oxidative phosphorylation system dysfunction in schizophrenia. International Journal of Molecular Sciences, 26(9), 5001. https://doi.org/10.3390/ijms26095001
Green, D. R., Galluzzi, L., & Kroemer, G. (2011). Mitochondria and the autophagy–inflammation–cell death axis in organismal aging. Science, 333(6046), 1109–1112. https://doi.org/10.1126/science.1201940
Hamblin, M. (2018). Mechanisms and mitochondrial redox signaling in photobiomodulation. Photochemistry and Photobiology, 94. https://doi.org/10.1111/php.12864
Harris, J. J., Jolivet, R., & Attwell, D. (2012). Synaptic energy use and supply. Neuron, 75(5), 762–777. https://doi.org/10.1016/j.neuron.2012.08.019
Huntington Study Group. (2024, June 21). Mitochondria dysfunction in Huntington’s Disease. Retrieved May 22, 2025, from https://huntingtonstudygroup.org/hd-insights/mitochondria-dysfunction-in-huntingtons-disease/
Kann, O., & Kovács, R. (2011). Mitochondria and neuronal activity. American Journal of Physiology-Cell Physiology, 301(6), C1207–C1219. https://doi.org/10.1152/ajpcell.00222.2011
Lin, M. T., & Beal, M. F. (2006). Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature, 443(7113), 787–795. https://doi.org/10.1038/nature05292
Kaur, H., Gugnani, K. D., & Reddy, P. H. (2025). Mitochondrial dysfunction in Alzheimer's disease. Ageing Research Reviews, 107, 102713. https://doi.org/10.1016/j.arr.2025.102713
Lopez-Domenech, G., Higgs, N. R., Vaccaro, V., Roš, H., Arancibia-Cárcamo, I. L., & Kittler, J. T. (2016). Loss of dendritic complexity precedes neurodegeneration in a mouse model with disrupted mitochondrial dynamics. Cell Reports, 17(2), 317–327. https://doi.org/10.1016/j.celrep.2016.08.073
Lopez-Otin, C., Blasco, M. A., Partridge, L., Serrano, M., & Kroemer, G. (2013). The hallmarks of aging. Cell, 153(6), 1194–1217. https://doi.org/10.1016/j.cell.2013.05.039
Ma, R., Li, S., & Zhang, Y. (2025). Mitochondrial dysfunction in neurodegenerative diseases: Mechanisms and corresponding therapeutic strategies. Journal of Molecular Neuropathology, 13(2), 327. https://doi.org/10.3390/jmn1302032
Magkouti, E., Leventakis, N., Alexandropoulou, A., Despoti, A., & Nanas, S. (2023). Quantitative EEG as outcome measure of the therapeutic effects of transcranial pho-tobiomodulation: A systematic review. Health & Research Journal. https://doi.org/10.12681/healthresj.30958
Neueder, A., Kojer, K., Gu, Z., Wang, Y., Hering, T., Tabrizi, S., Taanman, J.-W., & Orth, M. (2024). Huntington's disease affects mitochondrial network dynamics predisposing to pathogenic mitochondrial DNA mutations. Brain, 147(6), 2009–2022. https://doi.org/10.1093/brain/awae032
Park, S., Lim, W., You, S., & Song, G. (2019). Ochratoxin A exerts neurotoxicity in human astrocytes through mitochondria-dependent apoptosis and intracellular calcium overload.. Toxicology Letters. https://doi.org/10.1016/j.toxlet.2019.05.021
Picard, M. (2024). “Mitochondria are more than powerhouses—They’re the motherboard of the cell.” Scientific American.
Picard, M., & McEwen, B. (2018). Psychological stress and mitochondria: A conceptual framework. Psychosomatic Medicine, 80, 126–140. https://doi.org/10.1097/PSY.0000000000000544
Schweingruber, C., Nijssen, J., Mechtersheimer, J., Reber, S., Lebœuf, M., O'Brien, N. L., Mei, I., Hedges, E., Keuper, M., Benitez, J. A., Radoi, V., Jastroch, M., Ruepp, M. D., & Hedlund, E. (2025). Single-cell RNA-sequencing reveals early mitochondrial dysfunction unique to motor neurons shared across FUS- and TARDBP-ALS. Nature communications, 16(1), 4633. https://doi.org/10.1038/s41467-025-59679-1
Škrobot, M., Blahovcová, E., Konkoľová, J., Lauková, M., Klobučníková, K., Čierny, D., & Tomášiová, M. (2024). Mitochondrial dysfunction in sporadic amyotrophic lateral sclerosis patients: Insights from high-resolution respirometry. Biomedicines, 12(6), 1294. https://doi.org/10.3390/biomedicines12061294
Wang, R., Yang, Y., & Chang, H. (2022). The SDF1-CXCR4 axis is involved in the hyperbaric oxygen therapy-mediated neuronal cells migration in transient brain ischemic rats. International Journal of Molecular Sciences, 23. https://doi.org/10.3390/ijms23031780
West, A. P., Shadel, G. S., & Ghosh, S. (2015). Mitochondria in innate immune responses. Nature Reviews Immunology, 15(11), 505–518. https://doi.org/10.1038/nri3850
White, R. D., Turner, R. P., Arnold, N., Bernica, A., Lewis, B. N., & Swatzyna, R. J. (2022). Treating severe traumatic brain injury: Combining neurofeedback and hyperbaric oxygen therapy in a single case study. Clinical EEG and Neuroscience, 53(6), 519–531. https://doi.org/10.1177/15500594211068255
Yusuf, A. P., Mfullaana, Z. B., & Nkuna, S. P. (2023). Mitochondria targeted nanoparticles for the treatment of mitochondrial dysfunction-associated brain disorders. Frontiers in Bioengineering and Biotechnology, 13, 1563701. https://doi.org/10.3389/fbioe.2025.1563701
About the Author

Fred Shaffer earned his PhD in Psychology from Oklahoma State University. He earned BCIA certifications in Biofeedback and HRV Biofeedback. Fred is an Allen Fellow and Professor of Psychology at Truman State University, where has has taught for 50 years. He is a Biological Psychologist who consults and lectures in heart rate variability biofeedback, Physiological Psychology, and Psychopharmacology. Fred helped to edit Evidence-Based Practice in Biofeedback and Neurofeedback (3rd and 4th eds.) and helped to maintain BCIA's certification programs.
Support Our Friends









Comments