5-Second Science: Diet and Exercise Aid Cancer Treatment
- BioSource Faculty
- Jun 3, 2025
- 6 min read
Updated: Aug 1, 2025

Open-Access Article
Dinas, P.C., Karaventza, M., Liakou, C., Georgakouli, K., Bogdanos, D., & Metsios, G.S. (2024). Combined efects of physical activity and diet on cancer patients: A systematic review and meta-analysis. Nutrients, 16(11), 1749. https://doi.org/10.3390/nu16111749
What Did They Study?
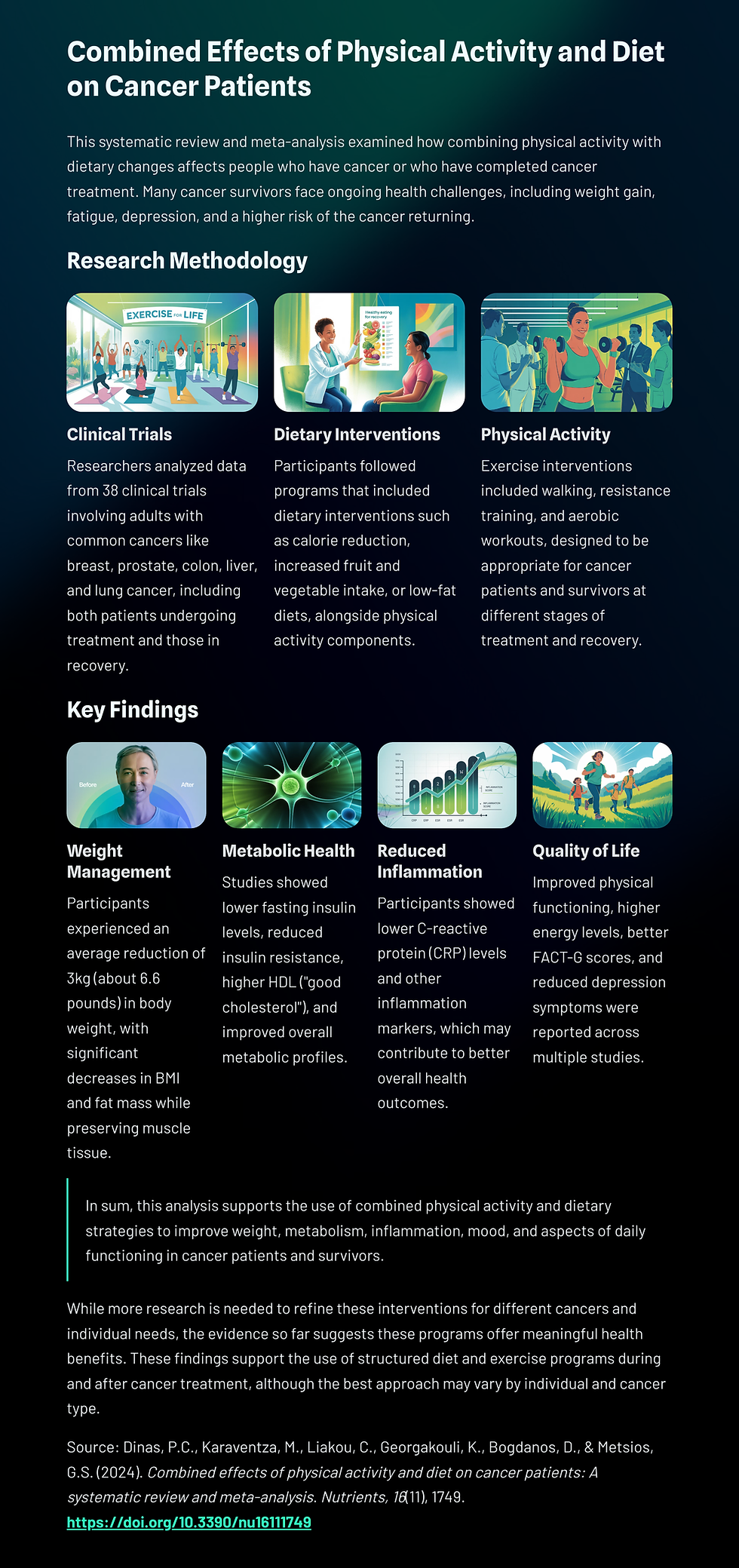
This systematic review and meta-analysis examined how combining physical activity with dietary changes affects people who have cancer or who have completed cancer treatment. Many cancer survivors face ongoing health challenges, including weight gain, fatigue, depression, and a higher risk of the cancer returning. While exercise and diet have each been studied separately, this research aimed to find out what happens when both are used together as part of a single program.
To answer this question, the researchers collected and analyzed data from 38 clinical trials involving adults with common cancers like breast, prostate, colon, liver, and lung cancer. Some people in these studies were still undergoing treatment, while others were in recovery. Across these trials, participants took part in programs that included physical activity—such as walking, resistance training, or aerobic workouts—and dietary interventions, such as calorie reduction, increased fruit and vegetable intake, or low-fat diets.
The goal was to see if these combined programs helped improve physical health (like weight, inflammation, and insulin levels), mental well-being (like depression), and quality of life (how patients feel and function day to day).
The results showed that people who participated in both diet and exercise interventions improved in several key areas compared to those who did not, suggesting these programs are a promising part of supportive care for cancer patients and survivors.
How Did They Do It?
The researchers followed a well-established process for gathering and analyzing scientific studies, using international guidelines to ensure their work was thorough and transparent. They searched several medical research databases—PubMed, EMBASE, and SportDiscus—without restricting the type of cancer, country, language, or publication date. This helped them capture as many relevant studies as possible.
They focused only on randomized controlled trials, which are considered the most reliable type of clinical research. These studies compared two groups: one group that received a combined diet and exercise program, and another group that did not (usually receiving standard care). To be included, studies had to report on measurable outcomes like body weight, blood markers (such as insulin or cholesterol), quality of life scores, or depression levels.
Once the relevant studies were selected, the research team assessed their quality using a tool called RoB2, which checks for things like bias and accuracy. Data from 30 of the 38 studies were combined in a meta-analysis—a statistical technique that pulls together results from multiple studies to find overall trends. When studies couldn’t be combined because they used different methods or reported different types of data, the authors summarized their findings in narrative form.
Finally, they rated the strength of the evidence for each outcome using a system called GRADE. This helped them judge whether the results were strong enough to support specific health recommendations. Despite some differences in study design and participant characteristics, the team concluded that these combined interventions offer real benefits for many cancer patients and survivors.
What Did They Find?
This comprehensive meta-analysis revealed that combining exercise with dietary changes leads to measurable health improvements for people diagnosed with cancer or recovering from treatment.
One of the clearest benefits was seen in weight-related outcomes: participants who followed both an exercise and nutrition program experienced reductions in body mass index (BMI), total body weight, and fat mass. On average, they lost nearly 3 kilograms (about 6.6 pounds) of body weight and about the same amount of body fat. These improvements were especially pronounced in individuals with breast cancer, although gains were observed across several cancer types.
In addition to weight loss, the interventions helped regulate blood sugar metabolism. Participants had lower levels of fasting insulin and reduced insulin resistance, measured using the HOMA-IR (homeostatic model assessment for insulin resistance). These changes suggest that their cells became more sensitive to insulin, which is a key protective factor in both cancer management and the prevention of cancer returning.
These metabolic improvements occurred without a significant loss in muscle mass among the intervention groups—an important consideration, since preserving lean body tissue is crucial for maintaining strength and health during cancer recovery.
The review also found reductions in C-reactive protein (CRP), a blood marker of chronic inflammation.
This suggests the interventions reduced the type of long-term inflammation that can contribute to cancer progression. These anti-inflammatory effects were most evident in breast cancer survivors, with less consistent results in those with prostate cancer.
Blood lipid profiles also improved. High-density lipoprotein (HDL), commonly known as “good cholesterol,” increased in participants, while triglycerides—fat molecules that, in excess, raise the risk of heart disease and cancer—decreased. These shifts signal a healthier metabolic state and are associated with better long-term outcomes.
Quality of life (QoL) measures were also assessed. Although there was no strong evidence that the interventions improved mental health scores, social functioning, or pain perception, participants did report feeling better physically. Measures such as physical functioning and energy levels improved, as did scores on a broader cancer-specific QoL assessment known as FACT-G (Functional Assessment of Cancer Therapy – General). These tools capture how well patients feel and function in daily life.
Lastly, the combined interventions led to a small but statistically significant reduction in depression symptoms. This finding is important, as depression is common among cancer patients and can worsen overall prognosis and daily functioning. The mood-lifting effects of exercise, likely due to increased brain endorphins, may be a major contributor to this improvement.
What Are The Implications For Cancer Treatment?
In sum, this analysis supports the use of combined physical activity and dietary strategies to improve weight, metabolism, inflammation, mood, and aspects of daily functioning in cancer patients and survivors.
While more research is needed to refine these interventions for different cancers and individual needs, the evidence so far suggests these programs offer meaningful health benefits.
Key Takeaways
A combination of physical activity and dietary change helps cancer patients and survivors reduce weight, body fat, and inflammation—factors linked to cancer progression.
These interventions improve metabolic health by lowering insulin levels and making the body more sensitive to insulin, which can reduce the risk of cancer recurrence.
Participants also showed improvements in cholesterol (higher HDL) and triglycerides, pointing to better overall cardiovascular and metabolic profiles.
While mental health scores didn't change significantly, patients reported feeling physically stronger and more capable, with a slight improvement in depression symptoms.
These findings support the use of structured diet and exercise programs during and after cancer treatment, although the best approach may vary by individual and cancer type.
Glossary
adiposity: the condition of being severely overweight or having an excessive amount of body fat.
C-reactive protein (CRP): a blood marker of systemic inflammation that is often elevated in cancer and linked to poor prognosis.
fat-free mass: the total mass of the body excluding all fat; includes muscle, bone, water, and organ tissue.
FACT-G (Functional Assessment of Cancer Therapy - General): a questionnaire assessing quality of life in cancer patients across physical, social, emotional, and functional well-being.
HOMA-IR (Homeostatic Model Assessment of Insulin Resistance): a method to estimate insulin resistance based on fasting glucose and insulin levels.
high-density lipoprotein (HDL): a form of cholesterol that helps remove other forms of cholesterol from the bloodstream; often called “good cholesterol.”
insulin resistance: a condition in which the body’s cells become less responsive to insulin, often leading to higher insulin levels and increased risk for type 2 diabetes and some cancers.
meta-analysis: a statistical technique that combines results from multiple studies to identify patterns and overall effects.
moderate-quality evidence: according to the GRADE system, evidence that is likely reliable but may be limited by factors such as bias or inconsistency.
physical component summary score: a metric from health-related quality of life assessments that focuses on physical health, including vitality, physical function, and pain.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses): a set of standards to improve the reporting of systematic reviews.
PROSPERO: an international database of prospectively registered systematic reviews.
resistance training: a type of physical activity involving weights or other resistance to build muscle strength and mass.
systematic review: a rigorous summary of research on a specific topic using a structured methodology to identify, appraise, and synthesize all relevant studies.
telomere: a region of repetitive nucleotide sequences at each end of a chromosome, whose length is considered a marker of cellular aging.
triglycerides: fat molecules found in the blood that serve as a major form of energy storage in the body. They are formed when the body converts excess calories, especially from carbohydrates, into fat.





Comments